Common OTC Medications: Uses, Side Effects, and Safety Tips You Need to Know

Every year, more than 80% of American adults reach for an over-the-counter (OTC) medication before calling their doctor. Whether it’s a headache, heartburn, or a stuffy nose, these pills and liquids are right there on the shelf - easy, fast, and seemingly harmless. But here’s the truth: OTC medications aren’t harmless. They’re powerful drugs, and using them wrong can land you in the emergency room.
What Exactly Are OTC Medications?
OTC medications are drugs approved by the FDA for use without a prescription. They’re meant for short-term relief of minor, self-diagnosable conditions like headaches, allergies, coughs, and indigestion. There are over 100,000 different OTC products on the market in the U.S., made from around 800 active ingredients. That means you’re not just buying "pain reliever" - you’re buying a specific chemical with specific risks.Think of them like tools. A hammer can build a house or break a window. Same with OTC meds. Take them as directed? They help. Take too much or for too long? They hurt.
Top OTC Medication Categories and How They Work
Not all OTC meds are the same. They fall into clear groups based on what they treat. Here’s what’s actually in your medicine cabinet - and what it’s really doing to your body.
Pain Relievers: Acetaminophen vs. NSAIDs
Two main players here: acetaminophen (Tylenol) and NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve).
Acetaminophen is the go-to for fever and mild pain. It doesn’t reduce inflammation, but it’s safer for people with stomach issues or bleeding disorders. The standard dose is 325-650 mg every 4-6 hours. Maximum daily dose? 4,000 mg. That’s just eight 500 mg tablets. Many people don’t realize that acetaminophen is in hundreds of combination products - cold medicines, sleep aids, even some prescription painkillers. Stack them up, and you can easily hit a toxic dose. The FDA estimates 15,000-18,000 cases of acute liver failure each year are linked to acetaminophen overdose.
NSAIDs like ibuprofen reduce pain, fever, and inflammation. That makes them better for sprains, arthritis, or menstrual cramps. But they irritate the stomach lining. Long-term use raises your risk of ulcers and internal bleeding. The maximum daily dose for ibuprofen is 1,200 mg for OTC use. Naproxen is stronger - only 660 mg per day. If you’re over 60, have high blood pressure, or take blood thinners, NSAIDs can be dangerous.
Cold and Flu: Decongestants, Cough Suppressants, and Expectorants
These are where things get messy. Most cold medicines are combo packs: decongestant + cough suppressant + antihistamine. That’s a problem.
Pseudoephedrine (Sudafed) shrinks swollen nasal passages. It works - but it can raise blood pressure and cause insomnia. That’s why it’s kept behind the pharmacy counter. You need to show ID and buy limited amounts.
Dextromethorphan (Delsym, Robitussin) suppresses coughs. Sounds harmless, right? But teens abuse it for its hallucinogenic effects at high doses. Emergency rooms see thousands of overdoses each year from this one ingredient.
Guaifenesin (Mucinex) thins mucus so you can cough it up. It’s safe, but only if you drink plenty of water. Otherwise, it does nothing.
Allergy Medications: Sedating vs. Non-Sedating
First-generation antihistamines like diphenhydramine (Benadryl) work fast - but they make you drowsy. Like, "can’t drive, can’t operate machinery" drowsy. They also cause dry mouth, blurry vision, and confusion in older adults. The JAMA Internal Medicine study found people over 65 who take Benadryl for sleep have a 30% higher risk of falling.
Second-generation options like loratadine (Claritin), fexofenadine (Allegra), and cetirizine (Zyrtec) are much better. They relieve sneezing, runny nose, and itchy eyes without the sleepiness. Doses are lower: 10 mg for loratadine, 180 mg for fexofenadine. But they still need caution. If you have kidney problems, your doctor may need to lower your dose.
Gut Issues: Antacids, H2 Blockers, and PPIs
Heartburn? You’ve got options.
Antacids like Tums (calcium carbonate) neutralize acid fast. Great for occasional burning. But if you take them daily, you risk kidney stones or electrolyte imbalances.
H2 blockers like famotidine (Pepcid AC) reduce acid production. They last longer than antacids. Safe for short-term use.
Proton pump inhibitors (PPIs) like omeprazole (Prilosec OTC) shut down acid production almost completely. They’re powerful - but they’re not meant for daily, long-term use. A 2023 JAMA study found people who take PPIs for more than a year have a 20-50% higher risk of chronic kidney disease. Don’t use them for months on end without seeing a doctor.
Diarrhea and Constipation
Loperamide (Imodium) slows your gut to stop diarrhea. It’s safe for most people - but not if you have a fever or bloody stool. That could mean infection, and stopping diarrhea could trap the bug inside. Also, people with kidney disease need lower doses.
For constipation, stool softeners like docusate are gentle. Stimulant laxatives like senna should only be used for a few days. Long-term use damages your colon’s natural function.
Who’s at Risk? The Hidden Dangers
OTC meds aren’t one-size-fits-all. Some groups are far more vulnerable.
Pregnant Women
ACOG says acetaminophen is the only safe pain reliever during pregnancy. NSAIDs like ibuprofen can cause serious kidney problems in the fetus after 20 weeks. Avoid them completely in the third trimester.
Children Under 4
The FDA banned cough and cold medicines for kids under 4 after 115 deaths between 1969 and 2006. That includes medicines with dextromethorphan, pseudoephedrine, or antihistamines. For fever or pain, use acetaminophen or ibuprofen - but only at the right weight-based dose. Never guess.
Adults Over 65
Older bodies process drugs slower. Diphenhydramine can cause confusion, urinary retention, and falls. Even loratadine may need a reduced dose if kidneys aren’t working well. Many seniors take multiple meds - and OTC drugs can interact with blood pressure pills, antidepressants, or blood thinners.
People with Chronic Conditions
If you have liver disease, skip acetaminophen. If you have kidney disease, avoid NSAIDs and adjust loperamide. If you have diabetes, check labels - some syrups are loaded with sugar. If you have asthma, NSAIDs can trigger attacks.
How to Use OTC Medications Safely
Here’s how to avoid the most common mistakes:
- Read the Drug Facts label - every time. It tells you the active ingredient, dose, warnings, and what not to mix it with.
- Don’t double up. If you’re taking a cold medicine, check if it already has acetaminophen or ibuprofen. Adding more = overdose.
- Know your limits. Acetaminophen max = 4,000 mg/day. Ibuprofen max = 1,200 mg/day. Naproxen max = 660 mg/day.
- Don’t use for more than 7-10 days. If symptoms don’t improve, see a doctor. OTC meds aren’t for chronic problems.
- Store safely. Keep them in a cool, dry place below 86°F. Check expiration dates. Old meds lose potency or can become unsafe.
- Ask your pharmacist. They’re trained to spot dangerous combinations. 93% of Americans live within 5 miles of a pharmacy. Use them.
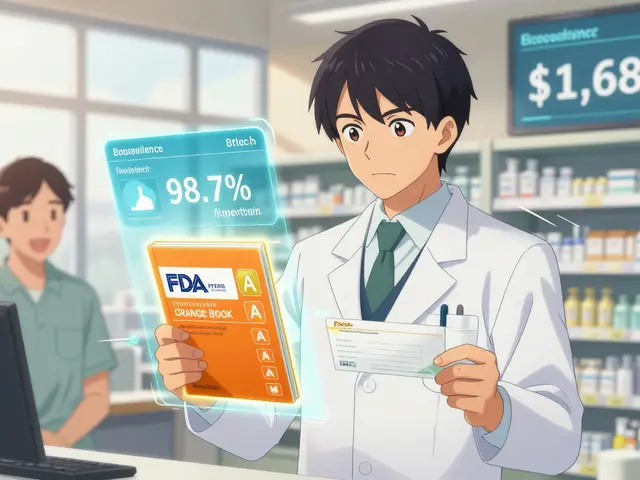
What’s Changing in OTC Medications?
The FDA just updated labeling rules. All OTC meds now must have a clear Drug Facts panel with exact doses and warnings. That’s good.
Some new options are now available without a prescription. Fluticasone furoate (Veramyst), a nasal spray for allergies, just lost its prescription status. That’s a win for people with chronic congestion.
Pharmacies are starting to offer pharmacist-led OTC consultations. CVS’s AI-powered "OTC Advisor" app scans your meds and flags risks. This is the future - personalized, safe self-care.
But the biggest threat? People treating chronic conditions like acid reflux or allergies with OTC meds for years. That’s not self-care. That’s self-harm.
When to Stop and See a Doctor
OTC meds are great - until they’re not. Call your doctor if:
- Pain lasts more than 10 days
- Fever stays above 102°F for more than 3 days
- Diarrhea or vomiting lasts more than 2 days
- You’re dizzy, confused, or have black stools
- You’re taking more than one OTC med at a time
- You’re pregnant, over 65, or have a chronic illness
Just because it’s on the shelf doesn’t mean it’s safe. Your body isn’t a lab. It’s a living system - and OTC meds can break it if you’re careless.
Can I take ibuprofen and acetaminophen together?
Yes, you can take them together if needed, as long as you stay within the daily limits for each. For example, you might take 650 mg acetaminophen and 200 mg ibuprofen at the same time for severe pain. But don’t do this daily without checking with your doctor. Mixing them doesn’t make them safer - it just gives you two ways to overdose.
Is it safe to use OTC meds for sleep?
Not really. Medications like diphenhydramine (Benadryl) or doxylamine (Unisom) cause drowsiness, but they’re not designed for long-term sleep. They can cause next-day grogginess, memory issues, and increase fall risk in older adults. If you need help sleeping, talk to your doctor about safer options like melatonin or behavioral changes.
What’s the difference between Claritin and Zyrtec?
Both are second-generation antihistamines and cause little to no drowsiness. Claritin (loratadine) is slightly less likely to cause drowsiness than Zyrtec (cetirizine), which can make some people sleepy. Zyrtec may work faster and stronger for severe allergies, but Claritin lasts longer. Try one, see how you feel, then switch if needed.
Can OTC meds damage my liver?
Yes - especially acetaminophen. Taking more than 4,000 mg in 24 hours can cause serious liver damage. Even lower doses can be dangerous if you drink alcohol, have liver disease, or take multiple products containing acetaminophen. Always check labels and never combine pain relievers without knowing what’s in them.
Are natural remedies safer than OTC meds?
Not necessarily. Herbal supplements like echinacea, garlic, or St. John’s wort aren’t regulated like drugs. They can interact with prescription meds, cause allergic reactions, or even harm your liver. Just because something is "natural" doesn’t mean it’s safe. Always treat supplements like medicine - research them and talk to your doctor.





Alexandra Enns
January 23, 2026 AT 21:46Oh please. You think Americans are the only ones dumb enough to treat OTC meds like candy? I’ve seen my cousin in Toronto pop 6 Advil at once because she had a "mild headache." And she wonders why her stomach is in ruins. This article is basically a kindergarten primer on common sense - and yet here we are. We need a national OTC literacy test just to buy ibuprofen. Seriously.
Marie-Pier D.
January 24, 2026 AT 12:42Thank you for writing this. 🙏 I’m a nurse and I see so many people come in with liver damage from stacking Tylenol with cold meds - and they’re always SO surprised. I keep a printed Drug Facts cheat sheet in my bag to hand out. If you’re reading this and you take more than one OTC med at once… please, please read the label. Your body isn’t a puzzle to solve - it’s your only one. 💛
blackbelt security
January 25, 2026 AT 19:35Good summary. I’ve trained soldiers on this stuff. The real danger isn’t the drugs - it’s the assumption that "if it’s on the shelf, it’s safe." That mindset gets people killed. Simple rules: one active ingredient at a time. No mixing. No guessing. If it doesn’t fix it in 3 days, see a doc. Done.
Patrick Gornik
January 26, 2026 AT 01:27Let’s deconstruct the epistemological fallacy embedded in the OTC paradigm: the illusion of autonomy masquerading as accessibility. The FDA, a regulatory apparatus steeped in pharmaceutical-industrial symbiosis, has commodified medical agency under the banner of "consumer sovereignty." But when you ingest pseudoephedrine for a stuffy nose, you’re not exercising freedom - you’re participating in a pharmacological performance art where your liver is the stage and your kidneys, the audience. The real question isn’t "how to use safely" - it’s why we’ve outsourced our somatic wisdom to corporate labeling. The answer? Capitalism. Always capitalism.
Tommy Sandri
January 27, 2026 AT 21:15This is a well-researched and appropriately cautious overview. The increasing prevalence of polypharmacy - even among OTC agents - warrants greater public health intervention. I would suggest that pharmacies implement mandatory counseling checkpoints for high-risk OTC purchases, particularly for individuals over 65 or those with chronic conditions. A standardized risk-assessment form, signed by the purchaser, could significantly reduce adverse events.
Juan Reibelo
January 28, 2026 AT 07:54Just wanted to add - if you’re taking anything with "PM" in the name, you’re taking diphenhydramine. That’s not sleep aid - that’s chemical sedation. I’m 58, and I used to take Unisom every night. Then I started forgetting where I put my keys. Then I fell in the shower. Then I stopped. Now I read. Or listen to audiobooks. Or stare at the ceiling. It’s not perfect. But it’s safer. And I haven’t forgotten my keys since.
Josh McEvoy
January 30, 2026 AT 01:16bro i took 3 advil and a tylenol cause my head was gonna explode and now i’m fine lmao 😎
venkatesh karumanchi
January 30, 2026 AT 20:00Really appreciate this breakdown. In India, people just grab whatever’s cheap and available - no labels, no warnings. I’ve seen grandmas take ibuprofen daily for back pain and wonder why they get dizzy. This info could save lives. Sharing with my family right now. 🙏
lorraine england
February 1, 2026 AT 07:04Ugh. So much of this is common sense, but apparently we’ve reached peak dumb. People think "natural" means safe? Have you heard of poison ivy? Or hemlock? Also, if you’re taking OTC meds for sleep, you’re not sleeping - you’re chemically numbing your nervous system. Go meditate. Or drink chamomile tea. Or go to bed at the same time. Radical, I know.
Kevin Waters
February 1, 2026 AT 09:29One thing this article misses: hydration. Most OTC meds - especially guaifenesin, NSAIDs, and even antacids - work better or are safer when you drink water. I always tell people: if you’re taking a pill, drink a full glass of water. It’s free, it’s simple, and it reduces side effects. Seriously, try it.
Kat Peterson
February 1, 2026 AT 19:37OMG I’m so glad someone finally said this. I used to take 2 Zyrtec a day because "it didn’t work" on 1. Then I realized I was basically sedated all day. I’m now on a $200/month prescription nasal spray and I’ve never felt more alive. Also, I don’t trust anything that doesn’t come in a glass bottle with a cork. 🫠✨