Control and Choice: How Autonomy in Medication Selection Empowers Patients

When you’re handed a prescription, do you feel like you’re making a decision-or just accepting one? For too many people, medication selection still feels like a one-way street: doctor recommends, patient takes. But that’s changing. Behind the scenes, a quiet revolution is underway in how patients and providers talk about drugs-not just what works, but what matters.
Why Your Right to Choose Medications Matters
Autonomy in medication selection isn’t just a buzzword from ethics textbooks. It’s the simple, powerful idea that you have the right to decide what goes into your body-even if your doctor disagrees. This isn’t about being difficult. It’s about respecting your life, your values, and your daily reality. Think about it: a pill you take every morning affects your sleep, your energy, your sex life, your wallet. It might make you nauseous, dizzy, or emotionally flat. No one else lives with those side effects. No one else carries the weight of paying for it month after month. So why should the decision be made without you? The legal and ethical foundation for this goes back decades. After the horrors of the Nuremberg Trials, medicine began to recognize that consent isn’t just a signature on a form-it’s an ongoing conversation. In 1972, the landmark Canterbury v. Spence case ruled that doctors must share all material risks. That means if a drug has a 1 in 4 chance of causing sexual dysfunction (as some antidepressants do), you deserve to know before you say yes. Today, 87% of U.S. healthcare institutions claim to support shared decision-making. But the gap between policy and practice is wide. In rural clinics, only 42% consistently involve patients in medication choices. And if you’re Black, Hispanic, or low-income, you’re far less likely to feel heard.What Real Medication Autonomy Looks Like
Autonomy doesn’t mean you get to pick the “best” drug based on a TikTok video. It means you get to pick the right drug for you. Here’s what that looks like in practice:- Knowing that SSRIs help 50-60% of people with depression-but 25-30% of those users face sexual side effects.
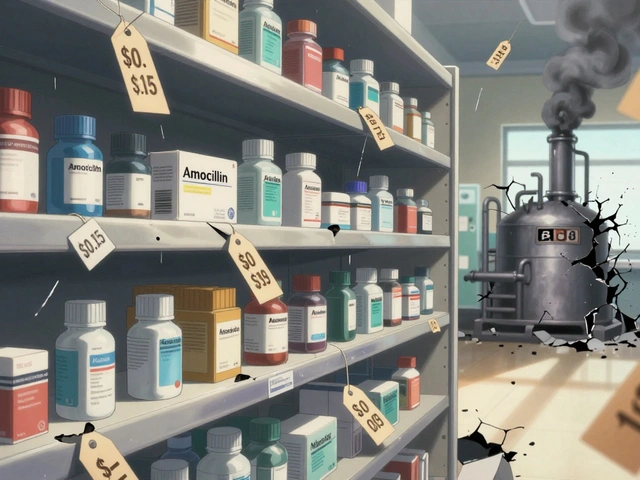
- Understanding that a brand-name biologic might cost $7,000 a month, while a biosimilar works just as well for $4,000.
- Being offered non-drug options: therapy, exercise, dietary changes, or digital tools like apps for anxiety or diabetes management.
- Having your doctor ask: “What matters most to you? Is it avoiding weight gain? Keeping your job? Not needing to take five pills a day?”
The Hidden Barriers to Choosing
You might think autonomy is just about knowledge. But it’s also about access, time, and trust. Most doctor visits last 15 minutes. That’s not enough to explain three different diabetes medications, their side effects, costs, and how each fits into your schedule, diet, and fears. A 2023 survey found 63% of patients felt rushed during medication discussions. Cost is another silent barrier. One in three Medicare Part D users changes or skips doses because of price. That’s not choice-that’s coercion. And if your doctor assumes you can’t afford a drug and doesn’t even mention it, that’s not autonomy. That’s paternalism dressed up as concern. Then there’s misinformation. Social media has fueled a 40% spike in antibiotic refusal requests, even when they’re medically necessary. But that doesn’t mean we should shut down patient questions. It means we need better tools-clear, simple, visual decision aids from trusted sources like the Mayo Clinic-to help people sort fact from fear. And let’s not forget cultural barriers. Many immigrants, elders, or people from collectivist cultures feel uncomfortable challenging authority-even when it’s their health on the line. Autonomy isn’t just about information. It’s about creating space where silence isn’t mistaken for agreement.
What Works: Real Stories, Real Change
One cancer patient refused opioids because of her religious beliefs. Her doctor didn’t push. Instead, they built a pain plan using non-opioid meds, nerve blocks, and acupuncture. She stayed in control. She stayed comfortable. Another patient, diagnosed with type 2 diabetes, was prescribed Ozempic. But she was terrified of nausea. Her doctor didn’t dismiss her. They showed her alternatives: metformin, GLP-1s with lower GI side effects, or even a structured weight-loss program. She chose a different GLP-1-and stayed on it for two years. Data backs this up. Patients who help choose their meds are 82% more likely to stick with them. That’s not magic. That’s respect. Meanwhile, pharmacies are stepping in. Medication Therapy Management (MTM) services-where pharmacists sit down with patients for 30-minute reviews-boost autonomy by 31%. These aren’t just refill check-ins. They’re conversations about what’s working, what’s not, and what else might fit.The Future Is Personalized, But Not Perfect
The next big leap? Personalization. Pharmacogenomic testing-analyzing your genes to predict how you’ll respond to a drug-is now under $250. In five years, it could be standard before prescribing. Digital tools are rising too. Apps that help you track side effects, compare costs, or even simulate how a drug might affect your daily life are gaining traction. But here’s the catch: 37% of adults over 65 struggle to use them. If we’re not careful, autonomy will become a privilege for the tech-savvy. New guidelines from the FDA and CMS are pushing systems to track patient preferences. By 2025, Medicare Advantage plans must document what medications patients want-or don’t want. That’s huge. It means your voice could be part of your medical record, not just a passing comment. But progress is uneven. Psychiatrists and endocrinologists lead the way, with over 70% practicing true shared decision-making. Emergency doctors? Only 43%. Why? Time, training, and culture. Changing that takes more than policy. It takes training.
How to Take Back Control
You don’t need to be a medical expert to advocate for yourself. Here’s how to start:- Ask: “What are my options besides this?” Don’t settle for “It’s the best one.”
- Ask: “What are the most common side effects-and how do they affect daily life?”
- Ask: “Is there a cheaper version? A generic? A non-drug alternative?”
- Ask: “How will this fit with my job, my family, my beliefs?”
- Bring a list of your concerns. Write them down before the appointment.
- Request a decision aid. Many clinics have printed or digital tools that compare options side by side.
- If you feel rushed, say so. “I need more time to think. Can we schedule a follow-up?”
Why This Isn’t Just About Drugs
Medication autonomy is really about dignity. It’s saying: You know your body better than any chart. Your life isn’t a clinical trial. Your choices aren’t mistakes-they’re data. When patients are truly involved, outcomes improve. Adherence rises. Hospitalizations drop. Trust grows. This isn’t about rejecting medical expertise. It’s about partnering with it. The best doctors don’t just prescribe. They listen. They adapt. They make space. The future of medicine isn’t about more pills. It’s about better conversations.Can I refuse a medication even if my doctor recommends it?
Yes. If you have decision-making capacity-meaning you understand the risks, benefits, and alternatives-you have the legal and ethical right to refuse any medication, even if your doctor believes it’s necessary. This is protected under informed consent laws and medical ethics guidelines. Your doctor should discuss why they recommend it, but they cannot force treatment. If they pressure you, you have the right to seek a second opinion or switch providers.
What if I can’t afford my prescribed medication?
Cost should never be a barrier to your right to choose. If a medication is too expensive, ask your doctor for alternatives: generics, biosimilars, patient assistance programs, or non-drug options. Many pharmaceutical companies offer discounts or free samples. Pharmacists can also help you find savings programs. Under Medicare Part D, you can request a formulary exception if your drug isn’t covered. You’re not alone-32% of Medicare beneficiaries adjust their meds due to cost, and your doctor should help you navigate that, not judge you for it.
How do I know if I have decision-making capacity?
Decision-making capacity means you can: understand the information given, appreciate how it applies to you, reason through the options, and communicate a clear choice. Most adults have this capacity unless they have severe dementia, acute psychosis, or are under extreme sedation. If there’s doubt, a simple tool called the Aid to Capacity Evaluation (ACE) can be used by clinicians. You don’t need a formal test to assert your right to choose-but if you’re unsure, ask for more time or bring a trusted family member to help you process the information.
Are there medications I can’t refuse?
In most cases, no. Even for serious conditions like diabetes or hypertension, you can refuse treatment. Exceptions exist only in emergencies where you’re unable to make decisions (like unconsciousness) or if you pose a direct danger to yourself or others (such as untreated psychosis with violent behavior). Even then, courts or ethics boards may be involved. For routine medications, refusal is always your right. The goal isn’t to override your choice-it’s to make sure you fully understand the consequences.
Why don’t more doctors talk about medication options?
Time, training, and system design. Most primary care visits are 10-15 minutes. Doctors are pressured to move quickly. Many weren’t trained in shared decision-making techniques. Electronic health records often don’t have fields to document patient preferences. And some providers still believe they know what’s best-especially if they assume a patient won’t follow through. But this is changing. New guidelines, patient demand, and tools like decision aids are pushing more providers to shift from telling to partnering.




ATUL BHARDWAJ
December 3, 2025 AT 03:55India too, we wait for doctor to speak. We nod. We pay. We take pill. No questions. But slowly, change coming. My aunt asked about cheaper medicine. Doctor smiled. Gave her generic. Small win.
Lynn Steiner
December 3, 2025 AT 21:42Ugh. Another self-help medical manifesto. 🙄 I’ve been on 7 different antidepressants. No one asked me what mattered. They just said ‘try this.’ I’m tired of being a lab rat.
Alicia Marks
December 4, 2025 AT 20:24You got this. Asking questions isn’t being difficult-it’s being smart. Write down your concerns before your next visit. You deserve to feel heard.
Paul Keller
December 6, 2025 AT 00:57While the premise of patient autonomy is philosophically sound, the practical implementation remains fraught with systemic inefficiencies. The physician-patient dynamic is not a marketplace; it is a clinical partnership predicated on expertise, not preference. The notion that a patient’s subjective values should supersede evidence-based protocols risks medical nihilism. Moreover, the 82% adherence statistic cited is correlational, not causal-confounding variables such as socioeconomic status and health literacy are not adequately controlled for in the referenced studies.
Jay Everett
December 6, 2025 AT 22:09Bro. I used to think my doc knew best. Then I found out my $800/month med had a $40 generic that worked just as well. I asked. He was kinda annoyed. But I saved $9k a year. Now I bring a list. I ask about side effects that mess with my sleep. I ask if therapy could help first. I don’t need a PhD to know what my body hates. 🤝
Steve Enck
December 7, 2025 AT 10:34One must question the epistemological foundation of this discourse. Autonomy, as framed here, is a liberal fantasy predicated on the myth of the rational agent. In reality, patients are emotionally vulnerable, cognitively overloaded, and culturally conditioned to defer to authority. To grant them ‘choice’ without addressing these structural incapacities is not empowerment-it is abdication. The real issue is not informed consent, but the collapse of clinical authority in the age of TikTok medicine.
मनोज कुमार
December 7, 2025 AT 23:00Doctor don't have time. Patient don't understand. System broken. End of story. Why waste energy on theory? Just take the pill. Save time.
Ella van Rij
December 9, 2025 AT 00:16Oh honey. Let me guess-you're the type who reads the FDA label and then writes a 12-page thesis on why your migraine meds are ‘ethically compromised.’ 🥱 I took Zoloft because my therapist said so. I cried every morning. I didn't ask about sex side effects because I assumed my doctor knew better. Turns out, she didn't. So now I Google. And I cry less. But I still hate the way my brain feels on SSRIs. Thanks for the article. Now I feel guilty for not being a better patient.
Joel Deang
December 10, 2025 AT 19:00my bro in la got his blood sugar down with just walking and lemon water. no meds. doctor was like ‘wow’ but then said ‘but we still gotta prescribe something for insurance.’ 😭 so yeah. autonomy? more like bureaucracy with a smile.
Arun kumar
December 11, 2025 AT 06:34in india we trust doctor. but now younger ones they ask us what we want. my dad changed his bp med after talking. he felt proud. maybe its not about power. just about being seen.
Zed theMartian
December 12, 2025 AT 10:38Of course you can refuse a pill. But if you refuse insulin and then collapse in the grocery store, who’s gonna pay for your ambulance? The state? Your family? Your ‘autonomy’ is just a fancy word for selfishness wrapped in a TED Talk. 🚨
Shannara Jenkins
December 13, 2025 AT 09:51My grandma finally asked her doctor about the cost of her heart med. He didn’t blink. He called a pharmacist on the spot. They found a coupon. She cried. It wasn’t about the money. It was about him listening. That’s the real win.
Elizabeth Grace
December 15, 2025 AT 09:00I just want to feel normal. Not be a medical case study. Why does every conversation feel like an interrogation? ‘Do you have concerns?’ ‘Are you sure?’ ‘Did you read the pamphlet?’ I just want to take the pill and go home.
Roger Leiton
December 15, 2025 AT 21:16Just had my first MTM session with my pharmacist. 30 mins. She asked about my sleep, my job stress, even my dog’s meds (he’s on heart pills too 😅). We cut my pill count from 8 to 5. I felt like a person, not a chart. 🙌
Laura Baur
December 17, 2025 AT 13:53Let’s be brutally honest: the entire ‘patient autonomy’ movement is a performative gesture designed to absolve healthcare systems of their responsibility to provide equitable, accessible care. When patients are forced to choose between insulin and rent, calling it ‘autonomy’ is not just misleading-it’s cruel. True autonomy requires not just information, but resources, time, cultural competence, and systemic support. Without these, you’re not empowering patients-you’re burdening them with the guilt of their own oppression.