Healthcare System Shortages: How Hospital and Clinic Staffing Crises Are Affecting Patient Care

When Hospitals Can’t Find Enough Nurses
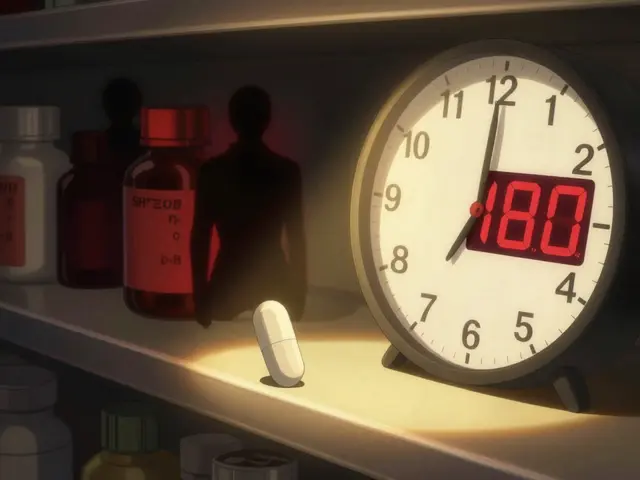
It’s 3 a.m. in a rural emergency room in Nebraska. The two nurses on duty are managing 12 patients - six in the ER, four waiting for beds, and two in triage with chest pain. One nurse just finished giving pain meds to a diabetic patient who’s been waiting over four hours. The other is calming down a family whose mother hasn’t seen a doctor in 18 hours. This isn’t a bad night. It’s Tuesday.
This isn’t an outlier. Across the U.S., hospitals and clinics are running on fumes. The number of open nursing positions hit 260,000 in late 2024, and more than 42 states are projected to face severe nursing shortages by 2030. It’s not just nurses. Doctors, mental health counselors, and even medical assistants are in short supply. The result? Longer waits, skipped care, and more mistakes.
Why the Shortage Is Worse Than Ever
The problem didn’t start with the pandemic, but the pandemic made it explode. Before 2020, hospitals were already struggling to hire enough staff. But then came the burnout. Nurses left in droves. In some units, turnover hit 104% - meaning more people quit than were hired in a single year. Many didn’t just change jobs. They left the profession entirely.
Why? Overwork. Underpay. Emotional exhaustion. Nurses in California report working 16-hour shifts with 3:1 patient ratios - meaning one nurse is responsible for three critically ill patients. In normal conditions, it’s 1:4 or 1:5. The American Nurses Association says this level of strain leads to a 7% higher death rate on units with too few staff. That’s not a statistic. That’s someone’s mother, father, or sibling.
And it’s not just hospitals. Rural clinics are even worse off. While urban clinics operate at about 79% staffing, rural ones are down to 58%. In places like Nevada or West Virginia, patients sometimes wait three days just to see a primary care provider. Some clinics have shut down their outpatient services entirely because they can’t find anyone to staff them.
The Domino Effect on Patient Care
When staff are stretched too thin, care suffers. It’s not always dramatic. Often, it’s quiet. A diabetic patient doesn’t get their insulin adjusted because the nurse didn’t have time. A senior with pneumonia gets sent home too early because the bed is needed for someone else. A child with asthma waits six hours in the ER because the doctor is stuck in another room.
Emergency rooms are hit hardest. The American College of Emergency Physicians found that understaffed ERs have 22% longer wait times than those with full teams. In 2024, Healthgrades reported a 27% jump in patient complaints about delays - many citing 72-hour waits for non-critical but urgent care. One mother in Arizona posted online: “My 4-year-old had a fever of 104. We waited 30 hours. By the time we saw a doctor, he was in septic shock.”
Medication errors are rising, too. Nurses who are working 12-hour shifts with no breaks are more likely to misread labels, miscalculate doses, or forget to check allergies. A 2022 JAMA study showed that for every 10% increase in nurse turnover, hospital-acquired infections rose by 6.5%. That’s not just a number. That’s someone getting sick because the system failed them.

Who’s Being Left Behind
Some groups feel the shortage more than others. Behavioral health services are in crisis. There are over 12,400 unfilled mental health positions nationwide - up 37% since 2023. People with depression, anxiety, or PTSD are waiting months for therapy. Some end up in ERs because there’s nowhere else to go.
Older adults are another group at risk. Nearly half of all nurses are over 50. One-third will retire in the next decade. Meanwhile, the number of Americans over 65 is growing fast - from 55 million today to 82 million by 2050. More seniors means more needs. More needs means more staff. But there aren’t enough new nurses coming in to replace those leaving.
Long-term care facilities are collapsing under the weight. They’re operating with 28% fewer nurses than before the pandemic. Residents are going without baths, turning in bed less often, and missing medication doses. In some cases, families report seeing their loved ones with bedsores because no one had time to reposition them.
Why Solutions Keep Failing
Hospitals have tried everything. They’ve raised wages. They’ve hired travel nurses. They’ve turned to AI tools and telehealth.
Travel nurses? They fill gaps - but at a cost. In 2023, travel nurses made up 12% of hospital staffing. But they cost 34% more than permanent staff. One ICU nurse in New York earned $185 an hour. Meanwhile, the hospital’s full-time nurses made $65. That created resentment, not relief.
AI tools sound promising. They can help with scheduling, documentation, even triage. But they’re not magic. It takes 8.7 weeks to train staff to use them properly. And 68% of hospitals can’t get their electronic records to talk to each other - so the tech doesn’t work. Plus, AI can’t comfort a scared patient or notice subtle changes in breathing.
States have tried laws. California mandates nurse-to-patient ratios. Other states are following. But without enough people to fill those roles, the rules just sit on paper. One hospital CEO in Texas said, “We’re legally required to have 1:4 ratios. We have 1:8. We’re breaking the law every shift.”

What’s Actually Working
Some places are finding real answers. The Mayo Clinic spent 18 months redesigning care teams. They gave nurses more control over their schedules, reduced paperwork with better tech, and created peer support groups. Result? Nurse turnover dropped by 31%.
Massachusetts cut its nursing shortage to 8% below the national average by offering full tuition reimbursement for nursing students who commit to working in-state for five years. That’s not a quick fix - but it’s sustainable.
Telehealth nurse triage helped reduce ER visits by 19% in pilot programs. A patient with a cough calls a nurse instead of driving to the ER. The nurse guides them through home care. It saves time, money, and stress.
But here’s the catch: none of these solutions work without investment. The American Medical Association says the U.S. spends $247 million a year on nursing education. They need $1.2 billion. That’s a gap of nearly $1 billion. And until that’s fixed, we’re just patching a leaky dam.
The Future Is Either Bright or Bleak
By 2030, the U.S. could be short 500,000 nurses. That’s half a million people who won’t be there to hold a hand, check a pulse, or catch a mistake before it’s too late.
There’s a path forward - but it’s hard. We need to pay nurses more. We need to fund nursing schools. We need to reduce paperwork. We need to give staff time to rest. We need to treat them like the professionals they are, not disposable cogs in a broken machine.
Right now, the system is running on guilt. Nurses stay because they care. But guilt isn’t a strategy. It’s not sustainable. And when the last nurse walks out, the patients will be left alone.
What You Can Do
If you’re a patient: Speak up. If you’re waiting too long, if you feel rushed, if you see staff overwhelmed - tell someone. Hospitals listen to complaints. Your voice matters.
If you’re a student: Consider nursing. It’s hard. But it’s needed. And there are scholarships, loan forgiveness, and support programs you can access.
If you’re a policymaker: Fund education. Raise wages. Protect staff. This isn’t a political issue. It’s a survival issue.
Healthcare isn’t just about drugs and devices. It’s about people. And right now, the people who keep us alive are running on empty.





Neil Ellis
January 22, 2026 AT 23:27And yeah, I know-‘just raise taxes’ or ‘hire more foreigners.’ But real change? It starts when we stop outsourcing compassion and start valuing the people who show up when no one else will.
My grandma’s last week? She had a nurse who sang her favorite hymns while changing her sheets. That’s not a job description. That’s love in scrubs.
Akriti Jain
January 23, 2026 AT 15:31Rob Sims
January 24, 2026 AT 08:09Meanwhile, the same people who cry about 'understaffing' are the ones who refuse to get a primary care doctor until their appendix bursts. You want better care? Stop treating the ER like a 24-hour Walmart pharmacy.
Mike P
January 25, 2026 AT 05:41And don’t get me started on the nurses who unionized and then demanded $100/hour while the rest of us are stuck with $18/hr jobs. Wake up. The system’s broken, but it ain’t because nurses are saints. It’s because we let bureaucrats turn healthcare into a performance art piece.
Fix the paperwork. Cut the red tape. Stop paying travel nurses triple. And for god’s sake, stop treating every patient like they’re the last person on Earth.
Daphne Mallari - Tolentino
January 26, 2026 AT 05:04One cannot sustain a professional class of caregivers when their labor is systematically devalued by market logic. The data is unequivocal: nurse-to-patient ratios correlate directly with mortality. Yet policy remains inert, constrained by ideological adherence to neoliberal orthodoxy.
What is required is not piecemeal reform but a paradigmatic reorientation toward care as a public good. Until then, we are merely arranging deck chairs on the Titanic.
arun mehta
January 27, 2026 AT 07:50What we lack is not compassion. We lack systemic support.
Perhaps the U.S. should learn that dignity isn’t found in wages alone, but in respect. And respect? It doesn’t come from headlines. It comes from listening. 🙏
Patrick Roth
January 28, 2026 AT 12:50Also, why is everyone acting like nurses are the only ones who work hard? My cousin works 12-hour shifts in a meatpacking plant. He doesn’t get a TED Talk. But okay, let’s keep the martyr complex going.
Lauren Wall
January 29, 2026 AT 10:31That’s the real crisis. Not the numbers. The silence.
Chiraghuddin Qureshi
January 31, 2026 AT 02:51Maybe the answer isn’t more money. Maybe it’s more heart. ❤️
Kenji Gaerlan
February 1, 2026 AT 11:31also i heard like 30% of them are just lazy and call in sick to go to disneyland? idk man just saying