Patient Information vs Healthcare Provider Information: How Label Differences Affect Your Care
Medical Term Translator
Understand Your Medical Record
Translate clinical terms you see in your records into plain language explanations. This tool helps bridge the gap between provider notes and patient understanding.
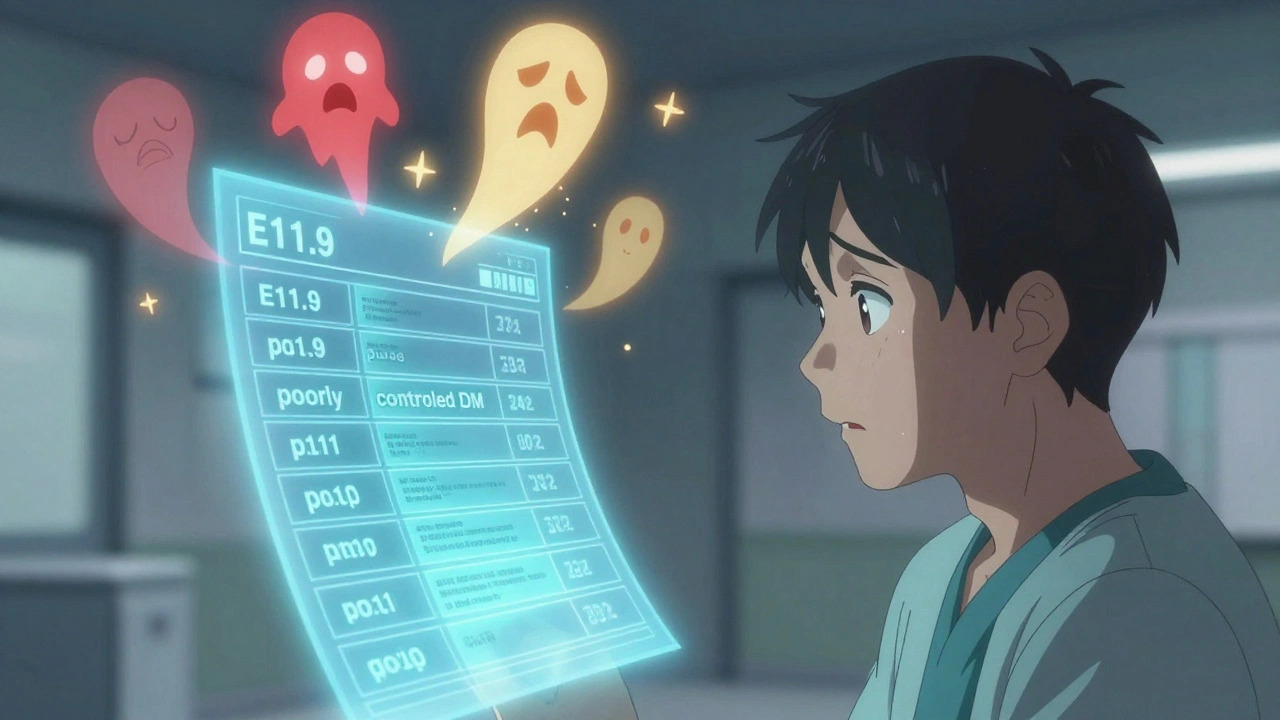
When you read your medical record and see "poorly controlled DM", do you think you’re being judged? Or do you think it means your blood sugar is too high? This isn’t just a misunderstanding-it’s a gap that’s been quietly hurting patient care for decades.
Healthcare providers write notes using a language built for efficiency, billing, and clinical precision. Patients experience illness in a completely different way-through fatigue, fear, confusion, and daily struggles. These two versions of the same story rarely match up. And when they don’t, it leads to mistakes, missed appointments, and even dangerous medication errors.
What’s Written vs. What’s Understood
Doctors use terms like hypertension, hyperlipidemia, or ICD-10 code E11.9 because those are the standardized codes required by insurance systems and electronic health records (EHRs) like Epic and Cerner. But patients don’t speak that language. In a 2019 study, 68% of patients didn’t understand common medical terms. Forty-two percent didn’t know hypertension meant high blood pressure. Sixty-one percent didn’t recognize colitis as an inflamed colon.
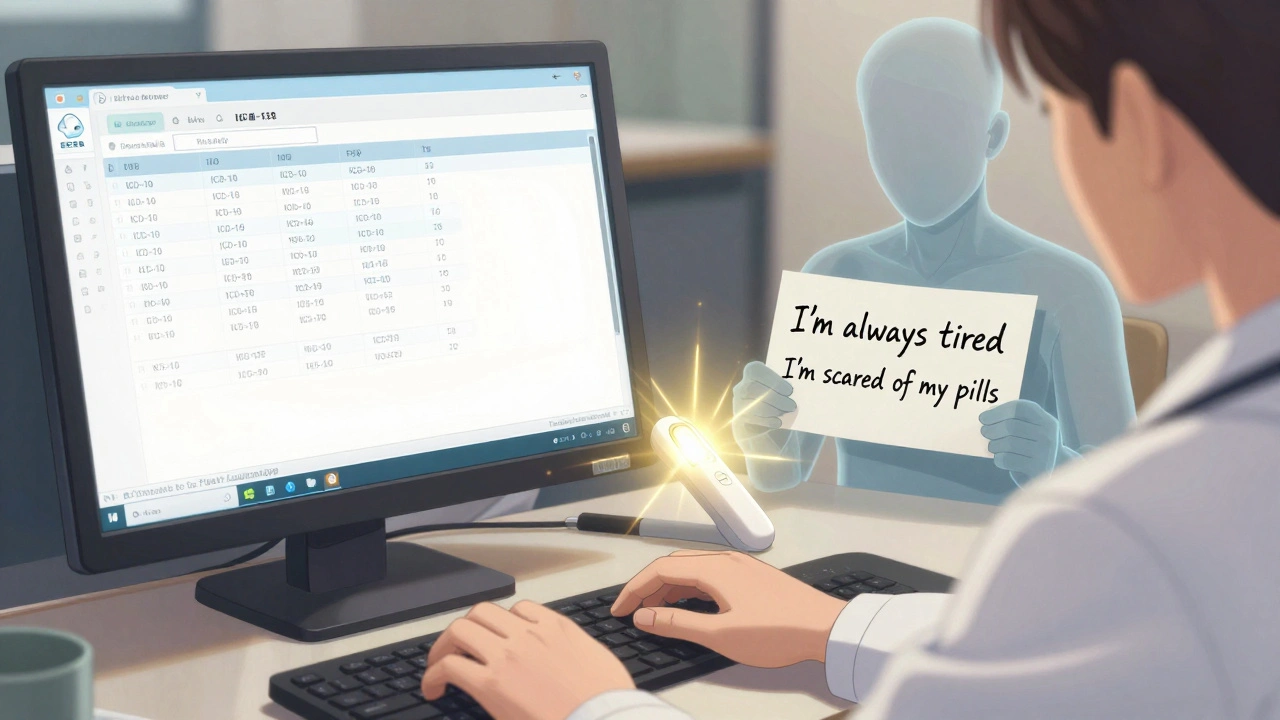
Meanwhile, patients describe their symptoms in plain, personal terms: "I’m always tired," "My feet feel numb," "I can’t sleep because my chest hurts." These aren’t just complaints-they’re vital clues. But if a provider doesn’t translate them into the system’s language, those clues get lost.
One patient on PatientsLikeMe wrote: "My doctor wrote 'poorly controlled DM' in my chart. I thought it meant I was a bad person." That’s not a failure of the patient. That’s a failure of the system.
Why the Labels Are So Different
Healthcare providers aren’t trying to confuse you. They’re following rules. Since 2015, U.S. hospitals have been required to use ICD-10-CM codes for every diagnosis. These codes are numbered, precise, and designed for billing and population health tracking. A single code like E11.9 stands for "Type 2 Diabetes Mellitus without complications." That’s useful for insurers and researchers-but it tells you nothing about how the patient feels.
On the patient side, there’s no official code for "I’m scared to take my pills because they make me dizzy." There’s no form to check for "I don’t understand why I need three different pills for the same problem." So those things go unrecorded in the system-until they cause a problem.
Meanwhile, the health information management (HIM) professionals who manage these records are trained to balance both worlds. They spend over 1,200 hours learning how to translate clinical notes into codes, while also protecting patient privacy under HIPAA. But they’re not always the ones talking to you during your visit.
The Real Cost of the Language Gap
This isn’t just about confusion-it’s about safety. Dr. Thomas Bodenheimer, a former professor at UCSF, found that miscommunication between patients and providers contributes to 30-40% of medication errors. That’s not a small number. That’s thousands of people each year taking the wrong dose, skipping doses, or stopping meds because they thought the doctor was blaming them.
A 2022 survey by the American Medical Association found that 57% of patients felt confused by the terms in their medical records. Thirty-two percent said they avoided follow-up care because of it. That’s not just bad for your health-it’s bad for the system. Hospitals now get paid based on how well patients report their experiences. The CMS HCAHPS survey includes questions like: "Did your providers explain things in a way you could understand?" If you say no, the hospital loses money.
And it’s not just patients who are frustrated. A 2023 Medscape survey showed 64% of physicians spend 15 to 30 minutes per visit just explaining basic terms. That’s time taken away from actual care.
What’s Being Done to Fix It
Some places are making real progress. Since 2010, Kaiser Permanente has let patients read their doctors’ notes through its "Open Notes" system. By 2021, they saw a 27% drop in patient confusion and a 19% increase in medication adherence. Patients weren’t just reading notes-they were understanding them.
Mayo Clinic built "plain language" templates into its EHR. When a doctor types "myocardial infarction," the system automatically shows "heart attack" in the version the patient sees. In their pilot program, patient confusion dropped by 38%.
The government is pushing too. The 21st Century Cures Act of 2016 made it illegal for providers to block patients from accessing their own records. By April 2021, every hospital had to let you see your clinical notes. And now, 89% of U.S. hospitals do-up from just 15% in 2010.
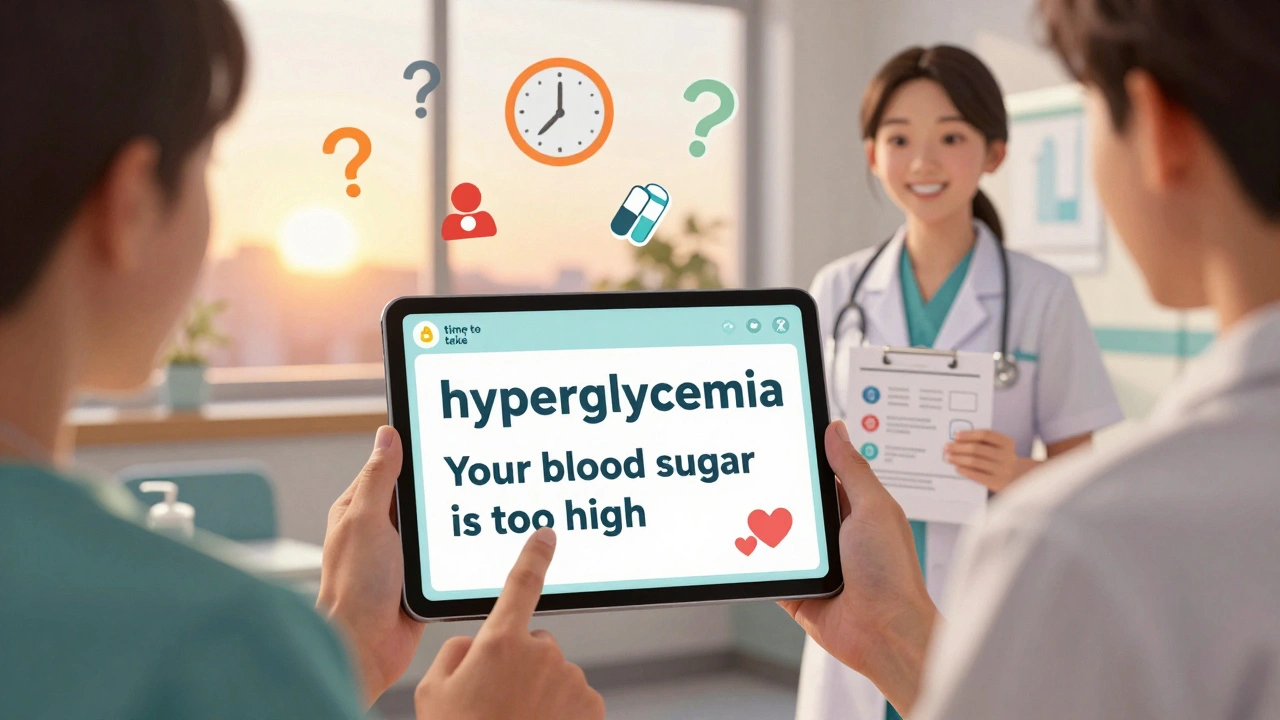
The World Health Organization’s ICD-11, rolled out in 2022, added patient-friendly descriptions alongside clinical codes for the first time. And new tech like Google Health’s Med-PaLM 2 can now convert clinical notes into plain language with 72% accuracy. It’s not perfect yet-but it’s getting closer.
What You Can Do Right Now
You don’t have to wait for the system to change. Here’s what works:
- Ask for plain language. After your doctor says "hypertension," say: "Can you say that in words I’ll understand?"
- Use the teach-back method. After they explain something, say: "So, just to make sure I got it-you’re saying I need to take this pill twice a day because my blood pressure is too high. Is that right?" This cuts misunderstandings by 45%, according to JAMA Internal Medicine.
- Read your notes. If your provider uses MyChart or another patient portal, log in and read your visit summary. If something sounds wrong or confusing, call and ask.
- Write down your symptoms in your own words. Before your visit, jot down: "What’s happening? When did it start? What makes it better or worse?" Bring that list. It helps your provider connect your story to their codes.
The Future Is Starting Now
By 2027, experts predict 60% of electronic health records will have real-time translation features-turning "hyperglycemia" into "your blood sugar is too high" on the spot. That’s not science fiction. It’s already being tested in pilot programs across major health systems.
The goal isn’t to replace medical terminology. It’s to make sure you’re not left out of the conversation. Your experience matters. Your words matter. And you have the right to understand what’s written about you.
The system isn’t perfect. But you’re not powerless. The more you ask, the more you read, and the more you speak up-the faster this gap closes. Because your health isn’t just a code in a database. It’s your life. And you deserve to understand it.





Jordan Wall
December 4, 2025 AT 03:11OMG this is such a critical issue lol 🤯 I mean, seriously-how is it that we’re still in 2024 and patients are expected to decode ICD-10 like it’s ancient Sumerian? 🤦♂️ I had a doc write ‘hyperlipidemia’ in my chart and I thought it meant I had a rare alien blood disorder. Turns out I just ate too many burritos. The system is broken, not me. #HealthcareFail
Gareth Storer
December 5, 2025 AT 17:23Oh wow, another feel-good article about how doctors are the villains here. Let me guess-the real problem is patients refusing to learn basic medical terms? Maybe if you spent less time Googling ‘is my headache a brain tumor’ and more time reading your discharge papers, you wouldn’t be so confused.
Jessica Baydowicz
December 7, 2025 AT 16:34Y’all. I literally cried reading this. 😭 My grandma died because she thought ‘diabetic neuropathy’ meant she was cursed. She stopped taking her meds because she thought the doctor was saying she was ‘bad’ for having it. This isn’t just jargon-it’s life or death. We gotta fix this. And yes, I’m calling my doc tomorrow to ask for plain language. No shame. No guilt. Just clarity.
Shofner Lehto
December 7, 2025 AT 23:24This is one of the most important pieces I’ve read all year. The disconnect between clinical documentation and patient experience isn’t a glitch-it’s a systemic failure. And the fact that 68% of patients don’t know what ‘hypertension’ means? That’s not ignorance. That’s negligence. We need mandatory plain-language training for every provider. Not optional. Not a suggestion. Required.
Yasmine Hajar
December 8, 2025 AT 15:10As a Black woman who’s been dismissed in ERs three times because I ‘sounded too articulate,’ I can tell you this language gap kills. They write ‘non-compliant’ when I say I can’t afford meds. They write ‘anxious’ when I’m scared they won’t believe me. This isn’t just about words-it’s about power. And we’re tired. But we’re not silent anymore. I print my notes. I highlight everything. I call back. And I make them say it again-in English.
John Filby
December 10, 2025 AT 00:39Just read my last EHR summary and realized my doctor wrote ‘poorly controlled DM’-and I thought it meant I failed some kind of moral test. I’m 32. I’ve had diabetes since I was 12. I’m not lazy. I’m exhausted. And now I know why I felt so guilty all these years. Thanks for putting this out there. I’m printing this and bringing it to my next appointment.
Emmanuel Peter
December 11, 2025 AT 19:25Let’s be real-this is just another excuse for patients to avoid personal responsibility. If you can’t understand ‘hypertension,’ maybe you shouldn’t be managing your own health. I’ve read my EHR since 2010. I know what ‘E11.9’ means. I take my meds. I track my glucose. You want clarity? Start by learning the damn language instead of blaming the system.
Ashley Elliott
December 13, 2025 AT 09:17...I think... this... is... important...
But... I... also... wonder... if... the... real... issue... is... that... we... expect... doctors... to... be... translators... AND... clinicians... AND... counselors... AND... billers...
...and... we... don’t... pay... them... enough... to... do... any... of... it... well...
...maybe... we... need... more... health... navigators...
...not... more... jargon...
...or... less... jargon...
...just... more... people... who... can... bridge... the... gap...
Augusta Barlow
December 13, 2025 AT 11:53Did you know the ICD-10 system was designed by insurance companies in the 90s to maximize billing and minimize payouts? And now they’re forcing doctors to use it? And now you’re telling patients to ‘read their notes’? That’s like telling a hostage to read the ransom note and ‘communicate better’ with their captors. This isn’t about language-it’s about control. The entire healthcare system is a profit-driven machine that treats people like data points. And they’re laughing all the way to the bank while you’re Googling ‘is this chest pain a heart attack or just anxiety?’
Chase Brittingham
December 13, 2025 AT 21:19I work in a clinic and I see this every day. One guy came in because his note said ‘non-adherent’-he didn’t know what that meant. He thought it meant he was a criminal. We sat down. I explained it. He cried. Then he asked if we could change the wording. We did. Simple. Human. It cost nothing. And it saved his trust. We need more of this. Not more tech. More humanity.
Bill Wolfe
December 15, 2025 AT 16:19Look, I’m a physician. I’ve been doing this for 22 years. I know the system is flawed. But let’s be honest-most patients don’t want to understand. They want a magic pill. They want someone else to fix it. They don’t want to learn the difference between ‘hyperlipidemia’ and ‘high cholesterol.’ They want to be told they’re ‘fine.’ And when they’re not? They blame the doctor. This isn’t a translation problem. It’s a cultural problem. And it’s not going away until patients stop treating healthcare like a customer service desk.
Benjamin Sedler
December 16, 2025 AT 08:01Wait-so you’re saying patients are confused because doctors use medical terms? What’s next? Should we stop using ‘heart attack’ and say ‘myocardial event’ instead? No, we should stop pretending patients need to understand everything. They just need to follow instructions. If they can’t, they need a caregiver. Not a dictionary.
zac grant
December 17, 2025 AT 22:50As someone who manages EHRs for a hospital, I’ve seen the transformation. The ‘Open Notes’ initiative? Game-changer. Patients who read their notes are 3x more likely to take meds correctly. And yes, it takes extra time. But the drop in readmissions? Worth it. The tech is coming. We’re training scribes to auto-translate notes in real time. It’s not perfect-but it’s moving. Keep asking. Keep reading. You’re part of the fix.
Carolyn Ford
December 19, 2025 AT 12:55They say ‘poorly controlled DM’ and you think you’re a bad person? Honey, you’re not the problem. The problem is that your doctor didn’t say ‘your blood sugar is too high’ because they’re lazy, overworked, and paid to code, not communicate. And now you’re supposed to be grateful they even wrote anything? This isn’t about education. It’s about accountability. Someone needs to get fired.
Heidi Thomas
December 20, 2025 AT 08:58Stop whining. Learn the words. Or don’t go to the doctor. Simple.