Shingles and Your Bones: How the Virus Impacts Bone Health
Shingles and Bone Health Risk Calculator
This tool estimates your risk of developing bone-related complications after a shingles outbreak based on key risk factors. Enter your information below to get personalized insights.
Your Risk Assessment
When a dormant varicella-zoster virus reactivates and causes a painful rash known as shingles, most people focus on the skin symptoms. Few realize that the virus can also mess with the skeletal system, leading to complications that linger long after the rash fades.
What Is Shingles and Why It Happens
Shingles is a reactivation of the chickenpox virus (varicella-zoster) that typically shows up as a unilateral band of blisters. After a childhood chickenpox infection, the virus hides in nerve tissue. Years or decades later, a weakened immune system can let the virus break free, traveling along nerves to the skin.
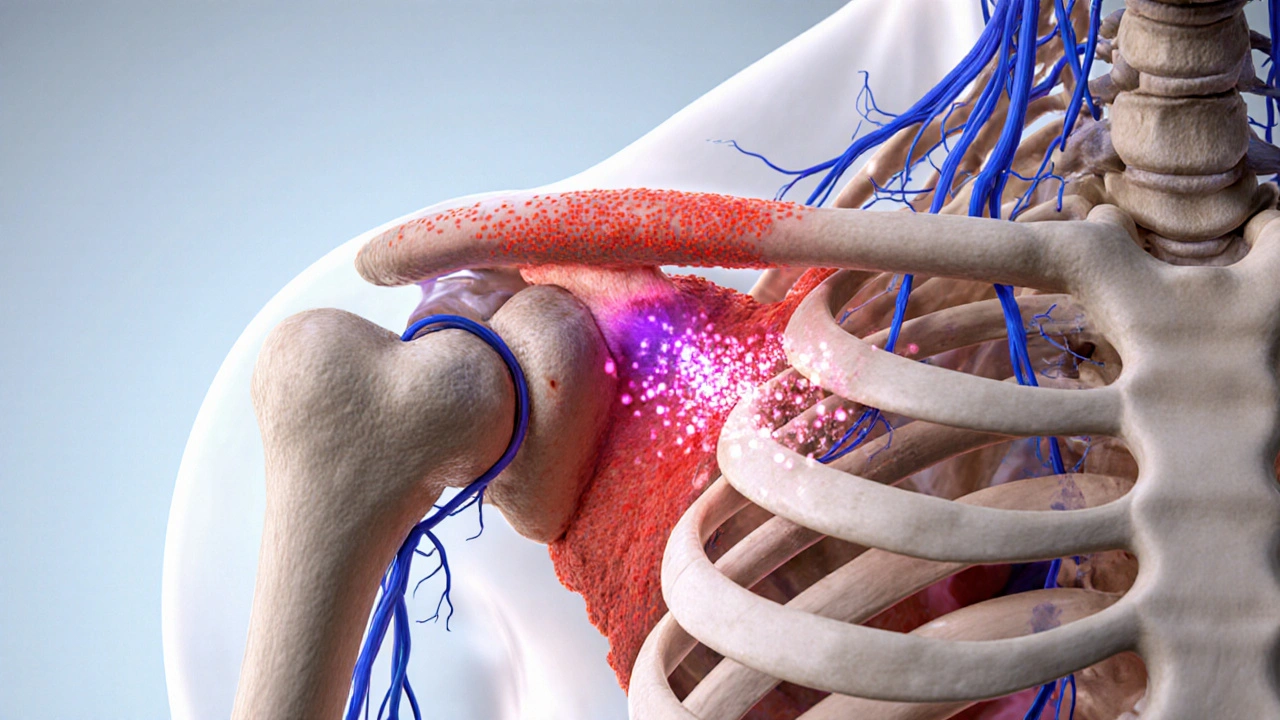
How Shingles Can Reach the Bones
Most shingles cases stay limited to skin and nerves, but three main pathways let the virus affect bone:
- Direct spread: In rare instances the virus travels from nerves to adjacent bone, causing osteomyelitis an infection of the bone tissue.
- Postherpetic neuralgia (PHN) aftermath: Persistent nerve pain can force patients to limit movement, leading to disuse osteoporosis.
- Inflammatory cascade: The intense inflammatory response can accelerate bone resorption, especially in older adults already at risk for osteoporosis.
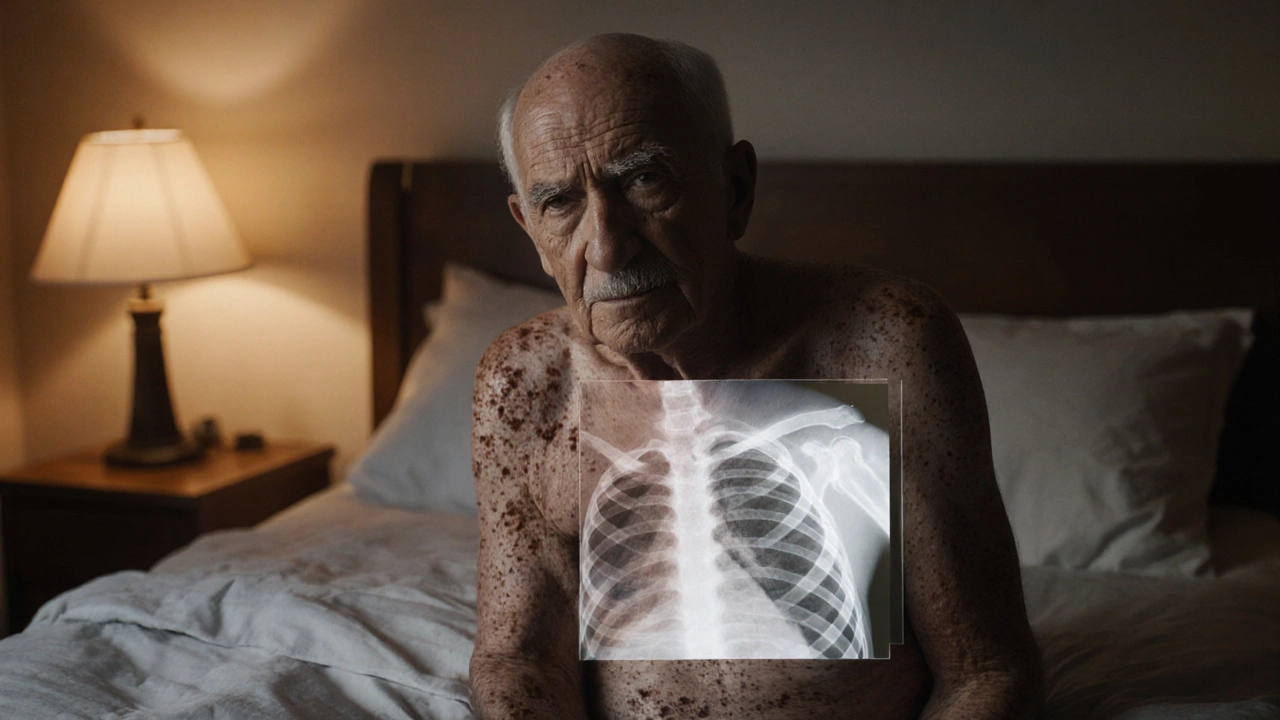
Spotting Bone‑Related Complications Early
Knowing the warning signs can prevent permanent damage. Watch for:
- Severe, localized pain that feels deeper than the rash area.
- Swelling or warmth over a joint or bone near the shingles belt.
- Fever that returns after the rash clears.
- Gradual loss of strength or stiffness in the affected limb.
If any of these pop up, a doctor may order an X‑ray, MRI, or blood test for inflammatory markers to rule out bone infection.
Treatment Options That Protect Both Skin and Skeleton
Prompt antiviral therapy is the cornerstone. Antiviral medication such as acyclovir, valacyclovir, or famciclovir shortens the rash and cuts down nerve damage risk. For bone involvement:
- Osteomyelitis: Requires a longer course of IV antibiotics, sometimes combined with surgical debridement.
- PHN‑related disuse: Physical therapy and low‑impact exercises keep bone density up. Calcium and vitamin D supplements are often recommended.
- Inflammation‑driven bone loss: Doctors may prescribe bisphosphonates or other osteoporosis meds if bone density tests show a drop.
Managing pain with gabapentin or pregabalin also helps patients stay active, reducing the risk of bone weakening.
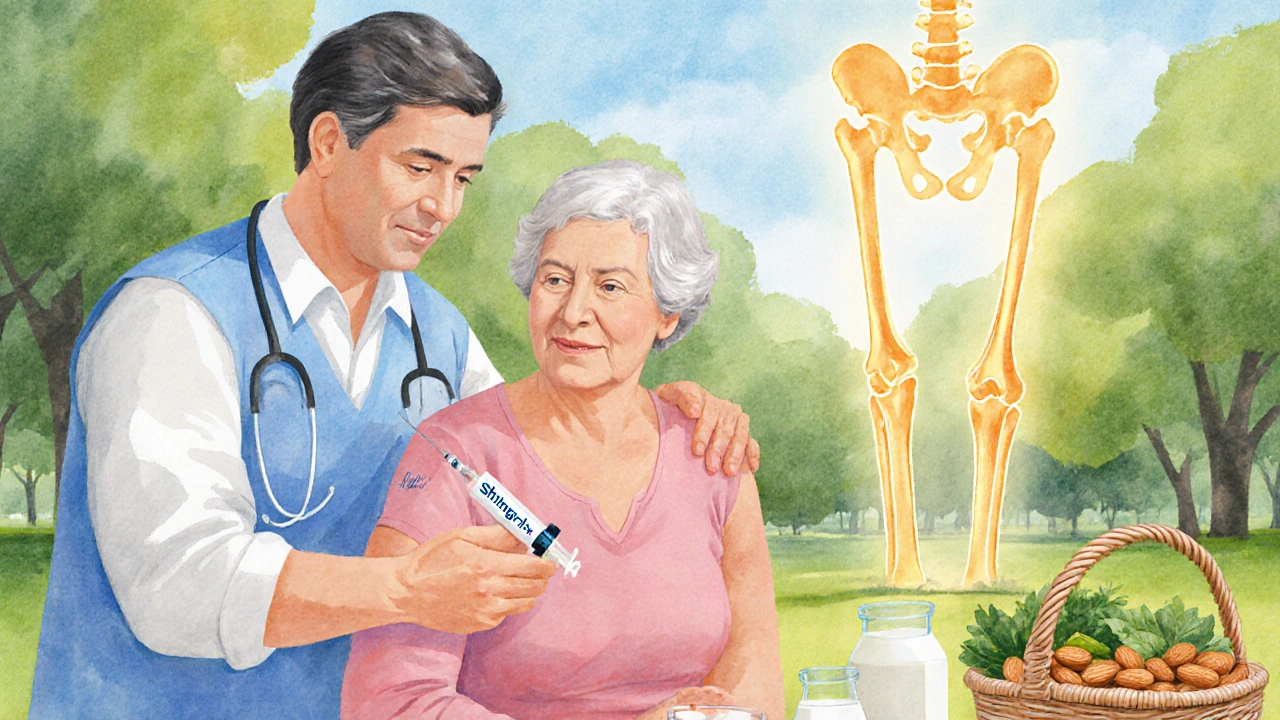
Preventing the Bone Fallout: Vaccines and Lifestyle Hacks
The most effective shield is vaccination. The shingles vaccine (Shingrix) is a two‑dose series that boosts immunity against varicella‑zoster. Clinical trials in 2023 showed a 97% reduction in shingles cases and a 90% drop in PHN, indirectly protecting bone health by keeping people mobile.
Beyond shots, keep your immune system in shape:
- Maintain a balanced diet rich in leafy greens, nuts, and lean protein.
- Aim for at least 150 minutes of moderate aerobic activity each week.
- Manage stress with mindfulness or light yoga-stress hormones can suppress immunity.
Comparison of Common Bone Complications After Shingles
| Complication | Typical Onset | Main Symptoms | Standard Treatment |
|---|---|---|---|
| Osteomyelitis | Within 2‑4 weeks of rash | Deep bone pain, fever, swelling | IV antibiotics ± surgery |
| Postherpetic neuralgia‑related disuse osteoporosis | Weeks to months after rash | Persistent nerve pain, reduced movement | Physical therapy, calcium/vit D, osteoporosis meds |
| Inflammatory‑mediated bone loss | 1‑3 months post‑infection | Generalized bone pain, decreased density on DEXA | Anti‑inflammatory drugs, bone‑strengthening agents |
When to Call Your Doctor
If you notice any of the red‑flag signs listed above, don’t wait for the rash to disappear. Early imaging and lab work can catch bone infection before it spreads. Ask your clinician about:
- Fast‑track referral to an infectious disease specialist if osteomyelitis is suspected.
- Bone density testing if you’ve been immobilized for more than two weeks.
- Adjusting antiviral dosage for immunocompromised patients.
Bottom Line: Protect Your Skin, Protect Your Skeleton
Shingles is more than a skin nuisance; its ripple effects can weaken the framework that holds you up. By understanding the shingles bone connection, getting vaccinated, treating the virus early, and staying active, you can dodge the hidden bone pitfalls.
Frequently Asked Questions
Can shingles cause permanent bone damage?
Yes, if the virus spreads to bone (osteomyelitis) or if severe postherpetic neuralgia leads to prolonged immobility, permanent damage or chronic osteoporosis can develop. Prompt treatment usually prevents lasting harm.
How common is osteomyelitis after shingles?
It’s rare, affecting roughly 1 in 1,000 shingles patients, but the risk rises in older adults, diabetics, and those with weakened immune systems.
Does the shingles vaccine protect my bones?
Indirectly, yes. By preventing shingles and especially postherpetic neuralgia, the vaccine reduces the chance of immobility‑related bone loss.
What lifestyle changes help after a shingles episode?
Start gentle range‑of‑motion exercises, maintain calcium‑rich nutrition, stay hydrated, and keep up with any prescribed antiviral or pain‑management regimen.
Should I get a bone density test after shingles?
If you experienced severe PHN, were immobilized for more than two weeks, or have other risk factors (age, menopause, steroid use), a DEXA scan is advisable.





Ujjwal prakash
October 5, 2025 AT 14:14Honestly, the connection between shingles and bone loss is more than a footnote, it’s a serious risk for anyone with a weakened immune system, especially if you’re over 70, have diabetes, or are on long‑term steroids, so keep an eye on that lingering pain!
Diane Helene Lalande
October 6, 2025 AT 04:07Thanks for the heads‑up, staying active can really help.
Edwin Levita
October 6, 2025 AT 18:00One must acknowledge the sheer drama of a virus that not only torments the skin but dares to infiltrate our very framework; the mere notion of shingles turning into osteomyelitis feels like a plot twist from a gothic novel, yet the clinical data backs it up.
Patients often underestimate how prolonged post‑herpetic neuralgia immobilizes them, paving the way for disuse osteoporosis.
Xander Laframboise
October 7, 2025 AT 07:54While the narrative is compelling, the evidence suggests that direct bone invasion is exceedingly rare; most bone complications stem from secondary effects like immobility, so let’s not overstate the danger.
Jason Petersen
October 7, 2025 AT 21:47Shingles rarely hits bones, the risk is minimal.
Melissa Gerard
October 8, 2025 AT 11:40Wow, downplaying a real threat? 🙄 Not everyone can just brush off bone loss like it’s a minor inconvenience.
Cindy Knox
October 9, 2025 AT 01:34Whoa, this is a game‑changer! If you thought shingles was just a rash, think again – your skeleton could be in the cross‑fire.
beverly judge
October 9, 2025 AT 15:27For anyone dealing with post‑herpetic pain, consider a gentle home‑based range‑of‑motion routine; even light stretching can preserve bone density while you recover.
Capt Jack Sparrow
October 10, 2025 AT 05:20Quick fact: antiviral therapy started within 72 hours cuts the chance of both PHN and subsequent bone complications by roughly 30 % according to recent meta‑analyses.
Manju priya
October 10, 2025 AT 19:14Remember, staying active isn’t just about muscles – it’s crucial for bone health; a daily 20‑minute walk can make a huge difference. 😊
Jesse Groenendaal
October 11, 2025 AT 09:07It’s ethically unacceptable to ignore how a preventable virus can silently erode the very structure that holds us up; we must demand broader vaccine coverage.
Persephone McNair
October 11, 2025 AT 23:00From a pathophysiological standpoint, the cytokine surge during VZV reactivation accelerates RANKL‑mediated osteoclastogenesis, which is the mechanistic basis for the observed bone demineralization.
siddharth singh
October 12, 2025 AT 12:54Let’s break this down step by step because the relationship between shingles and bone health is often oversimplified, leading many patients to underestimate the seriousness of the condition.
First, the varicella‑zoster virus lies dormant in dorsal root ganglia and can reactivate when cellular immunity wanes, typically in older adults or immunocompromised individuals.
When reactivation occurs, the virus travels along sensory nerves to the skin, producing the classic painful rash.
However, the nerve inflammation does not stay confined to the skin; it can spill over into adjacent musculoskeletal structures, particularly when the rash follows a dermatomal distribution that overlays bony prominences such as the thoracic vertebrae or ribs.
In rare but clinically significant cases, the virus can directly infect bone tissue, resulting in osteomyelitis, a condition that requires aggressive intravenous antibiotics and sometimes surgical debridement.
More commonly, the intense, lingering pain known as post‑herpetic neuralgia (PHN) forces patients into prolonged periods of reduced mobility.
This disuse leads to accelerated bone resorption through decreased mechanical loading, a phenomenon well documented in orthopedic literature as disuse osteoporosis.
Additionally, the inflammatory cascade triggered by VZV releases cytokines such as IL‑1, IL‑6, and TNF‑α, which stimulate osteoclast activity and suppress osteoblast function, further tipping the balance toward bone loss.
Age‑related bone density decline synergizes with these processes, meaning that an elderly patient who develops shingles is at a compounded risk for fractures.
Clinically, physicians should watch for red‑flag signs: deep, localized bone pain beyond the rash, swelling, warmth, or recurrent fevers after the rash resolves, as these may herald osteomyelitis.
If such symptoms appear, prompt imaging-starting with X‑ray, followed by MRI if needed-and laboratory work for inflammatory markers are essential.
Treatment must be two‑pronged: antiviral therapy (e.g., valacyclovir) to curb viral replication, and targeted management of bone complications, which may include a course of IV antibiotics for osteomyelitis, bisphosphonates or denosumab for rapid bone loss, and a structured physical therapy regimen to restore mechanical loading.
Adjunctive pain control with gabapentinoids can also improve patient mobility, indirectly protecting bone health.
Prevention is paramount; the recombinant shingles vaccine (Shingrix) has shown >90 % efficacy in preventing both shingles and PHN, thereby indirectly safeguarding the skeleton.
Coupled with lifestyle measures-adequate calcium and vitamin D intake, weight‑bearing exercise, and smoking cessation-the risk of bone complications can be dramatically reduced.
Angela Green
October 13, 2025 AT 02:47Minor note: "antiviral therapy" should be capitalized only when starting a sentence; also, avoid the double space before "and" in the last sentence.
April Malley
October 13, 2025 AT 16:40Great summary! This definitely helps me understand why staying active after shingles matters for bone health.
scott bradshaw
October 14, 2025 AT 06:34Sure, because the government really cares about your bones.
Crystal Price
October 14, 2025 AT 20:27Honestly, I think most people just need to get the vaccine and stop worrying about bone stuff.
Murhari Patil
October 15, 2025 AT 10:20Did you know that the vaccine is actually a covert way to track DNA? That's why bone health gets mentioned – it's all part of the plan.