How Post‑Surgery Eye Inflammation Triggers Ocular Migraines

Ocular Migraine vs. Post-Surgery Inflammation Symptom Checker
Symptom Assessment Tool
Answer these questions to help determine if your symptoms are likely post-surgery inflammation or an ocular migraine. Based on the article's key differences.
Quick Summary
- Postoperative eye inflammation can set off an ocular migraine by altering blood flow and nerve signaling.
- Key culprits are prostaglandins, inflammatory cytokines, and spikes in intraocular pressure.
- Common procedures linked to this risk include cataract surgery and LASIK.
- Early use of NSAIDs or corticosteroid eye drops can cut the migraine trigger in half.
- Seek urgent care if visual aura or severe headache persists after eye surgery.
Understanding Postoperative Eye Inflammation
When you undergo any eye operation, the tissue around the incision reacts like it would after a cut or bruise. This natural response is called postoperative eye inflammation a temporary swelling that involves blood vessels, immune cells, and fluid buildup in the ocular tissues. The body releases chemicals such as prostaglandins and cytokines to start healing, but if those signals stay high for too long, they can irritate nearby nerves.
What Is an Ocular Migraine?
An ocular migraine a visual disturbance that often begins with a flickering or scintillating aura, followed by a headache that may affect one side of the head is different from a classic migraine. The hallmark is a temporary loss of vision, flashing lights, or zig‑zag patterns that usually last 20‑30 minutes. While the aura is the eye’s way of warning you, the subsequent headache can be intense and is often accompanied by nausea or light sensitivity.

How Inflammation Sets Off an Ocular Migraine
The link isn’t magic-it’s biochemical.
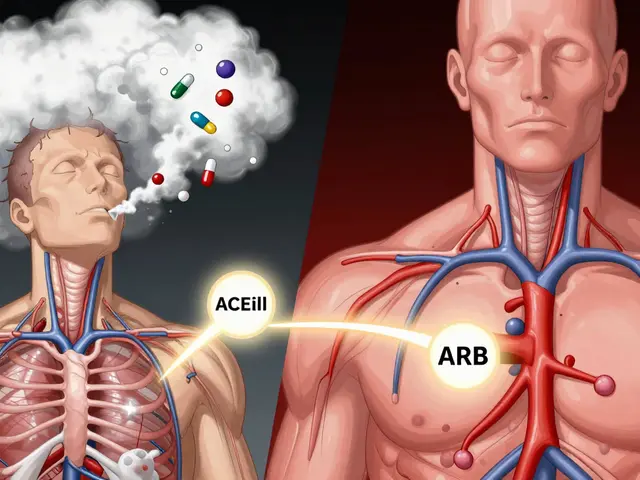
- Prostaglandins - After surgery, prostaglandins lipid compounds that amplify pain and increase blood vessel permeability surge. High levels make the tiny vessels in the retina more leaky, which can trigger the visual aura.
- Inflammatory cytokines - Molecules like interleukin‑6 and tumor necrosis factor‑α act as messengers that tell nerves to fire more aggressively. When they linger, the trigeminal nerve (the main migraine conduit) becomes hypersensitive.
- Intraocular pressure spikes - Swelling compresses the eye’s fluid channels, leading to a temporary rise in intraocular pressure the fluid pressure inside the eye that normally stays around 10‑21 mmHg. Even a modest increase can squeeze retinal vessels, provoking the aura.
- Vasospasm - Inflammation can cause the blood vessels supplying the optic nerve to contract briefly, cutting off oxygen. The brain interprets this as a migraine trigger.
Put together, these factors turn a normal healing process into a migraine‑setting environment.
Surgeries Most Often Associated with This Phenomenon
Not every eye operation carries the same risk. Here are three that show the strongest connection.
- cataract surgery removal of the clouded lens followed by insertion of an artificial intraocular lens. The incision and phacoemulsification generate significant fluid turbulence, raising inflammation markers.
- LASIK laser‑assisted in‑situ keratomileusis that reshapes the cornea to correct refractive errors. While the flap is thin, the high‑energy laser can provoke a cytokine surge.
- retinal detachment repair procedure that reattaches the retina using laser or cryotherapy, often followed by gas or silicone oil tamponade. The intra‑ocular tamponade adds pressure, amplifying the intraocular pressure spike.
Spotting the Difference: Inflammation vs. Ocular Migraine
| Feature | Post‑Surgery Inflammation | Ocular Migraine |
|---|---|---|
| Onset | Within 24‑48hours | Usually 2‑72hours after surgery |
| Visual aura | Rare, usually just haziness | Flashing lights, zig‑zag patterns |
| Pain type | Dull ache, pressure sensation | Pulsating headache, often unilateral |
| Response to NSAIDs | Quick relief | Partial; may need migraine‑specific meds |
| Associated signs | Redness, tearing, photophobia | Photophobia, nausea, phonophobia |
This side‑by‑side view helps you decide whether you’re dealing with plain swelling or a migraine that needs extra attention.
Prevention and Early Management
Stopping the chain reaction early is the smartest move.
- **Prophylactic NSAID drops** - Prescribed as ketorolac 0.4% or bromfenac 0.09% immediately after surgery, they cut prostaglandin production by up to 60%.
- **Short‑course corticosteroids** - A tapered regimen of prednisolone acetate 1% for 3‑5 days dampens cytokine storms without raising intra‑ocular pressure.
- **Carbonic anhydrase inhibitors** - Medications like brinzolamide can lower intra‑ocular pressure spikes when used for a week post‑operation.
- **Hydration and diet** - Staying well‑hydrated and limiting caffeine reduces vascular sensitivity.
- **Scheduled follow‑ups** - A day‑one and week‑one check‑up catches lingering inflammation before it sparks a migraine.
If a visual aura appears, log the time, duration, and any accompanying headache. This record helps your ophthalmologist decide whether to add a migraine‑specific drug such as rizatriptan.
When to Call Your Eye Doctor
Don’t wait for the next scheduled visit if you notice any of these red flags:
- Vision loss lasting longer than 30minutes.
- Severe, throbbing headache that doesn't ease with OTC pain relievers.
- Sudden increase in eye redness or swelling.
- New onset of double vision or eye movement pain.
Prompt treatment can prevent a short‑lived aura from turning into a chronic migraine pattern.
Frequently Asked Questions
Can every eye surgery cause ocular migraines?
No. The risk is highest with procedures that provoke strong inflammatory responses-cataract extraction and retinal repairs top the list. Simple refractive adjustments, like laser capsulotomy, rarely trigger migraines.
Do over‑the‑counter painkillers help?
Ibuprofen or naproxen can ease the pressure‑type pain of inflammation, but they often fall short of stopping the visual aura. For that, a migraine‑targeted medication prescribed by a doctor is usually needed.
Is it safe to use both NSAID eye drops and oral NSAIDs together?
Yes, most surgeons approve combined therapy because the topical drops act locally while oral NSAIDs reduce systemic inflammation. Just follow the dosage guidelines to avoid stomach irritation.
How long does an ocular migraine last after surgery?
The visual aura typically fades within 20‑30 minutes, but the headache can linger for up to 2hours. If symptoms persist beyond 4hours, seek medical advice.
Can lifestyle changes reduce the risk?
Absolutely. Regular sleep, limiting caffeine, staying hydrated, and managing stress are proven to lower both postoperative inflammation and migraine susceptibility.



Krishna Chaitanya
October 15, 2025 AT 15:34Dude this eye‑migraine thing is insane!
diana tutaan
October 16, 2025 AT 13:47The article correctly identifies prostaglandins as a key trigger. Reducing them with NSAID drops cuts the risk significantly. Early intervention is essential to prevent prolonged aura.
Sarah Posh
October 17, 2025 AT 12:01Thanks for breaking that down. It’s good to know that a simple drop can make a big difference for patients. Keep spreading the info!
James Knight
October 18, 2025 AT 10:14Sure drama sells clicks but the science is solid. No need to overreact.
Ajay D.j
October 19, 2025 AT 08:27In many Indian clinics they already use prophylactic NSAID drops after cataract surgery. It’s a habit that could help reduce these migraines globally.
Dion Campbell
October 20, 2025 AT 06:41One must commend the author for venturing into a topic that sits at the intersection of ophthalmology and neurology.
However, the exposition suffers from a lamentable lack of depth regarding the molecular cascade.
Prostaglandins, for instance, are not merely mentioned in passing but deserve a thorough mechanistic discussion.
The reader is left to infer how cyclooxygenase inhibition translates into vascular stability within the retina.
Moreover, the brief nod to intra‑ocular pressure spikes omits the nuanced role of aqueous humor dynamics.
A seasoned clinician would appreciate a more elaborate quantitative analysis of pressure thresholds.
The inclusion of a solitary hyperlink does little to substantiate the sweeping claims made.
One expects a review of primary literature, not a cursory summary of secondary sources.
Furthermore, the recommendation of NSAID eye drops, while sensible, is presented without acknowledgment of contraindications.
Patients with a history of gastric ulcers, for instance, may experience adverse systemic effects.
The author also neglects to address the potential of corticosteroid‑induced ocular hypertension.
Such omissions are not trivial; they bear directly on clinical decision‑making.
In addition, lifestyle modifications are cited, yet the advice remains generic and lacks actionable specifics.
A more refined piece would integrate dietary guidelines, sleep hygiene, and stress‑management techniques.
In sum, while the article provides a useful overview, it falls short of the scholarly rigor demanded by the field.
Burl Henderson
October 21, 2025 AT 04:54The point about cyclooxygenase pathways is spot on, and the pressure dynamics deserve deeper dive. Integrating those data points could enhance protocol optimization.
Leigh Ann Jones
October 22, 2025 AT 03:07I’ve read the piece a couple of times and while the baseline info is solid, the flow feels disjointed. The sections jump from inflammation biochemistry straight to lifestyle tips without a smooth transition, which can confuse readers. Also, the table comparing symptoms is useful but could be formatted better for quick scanning. The recommendation list is comprehensive yet repeats the same idea of NSAID drops in different wording. Overall, it’s a decent primer but could benefit from tighter editing and clearer sub‑headings.
Robert Brown
October 23, 2025 AT 01:21Sounds like you just needed an editor.