Adrenal Insufficiency from Corticosteroid Withdrawal: How to Recognize and Manage It

Steroid Taper Calculator
How to Use This Tool
This calculator helps determine the appropriate tapering schedule for corticosteroids based on your current dose and duration of use. It follows evidence-based guidelines from the Endocrine Society and European Society of Endocrinology.
Stopping corticosteroids like prednisone or dexamethasone suddenly can trigger a life-threatening condition called adrenal insufficiency. It’s not rare. In fact, about 1 in 30 adults in the U.S. is on these drugs at any time, and many don’t know the risks of quitting cold turkey. Even short courses-like a two-week steroid pack for a bad sinus infection-can mess with your body’s natural cortisol production. When you stop, your adrenal glands, which have been shut down by the medication, can’t snap back fast enough. The result? Fatigue so deep it feels like your bones are made of lead, nausea, low blood pressure, and sometimes, shock.
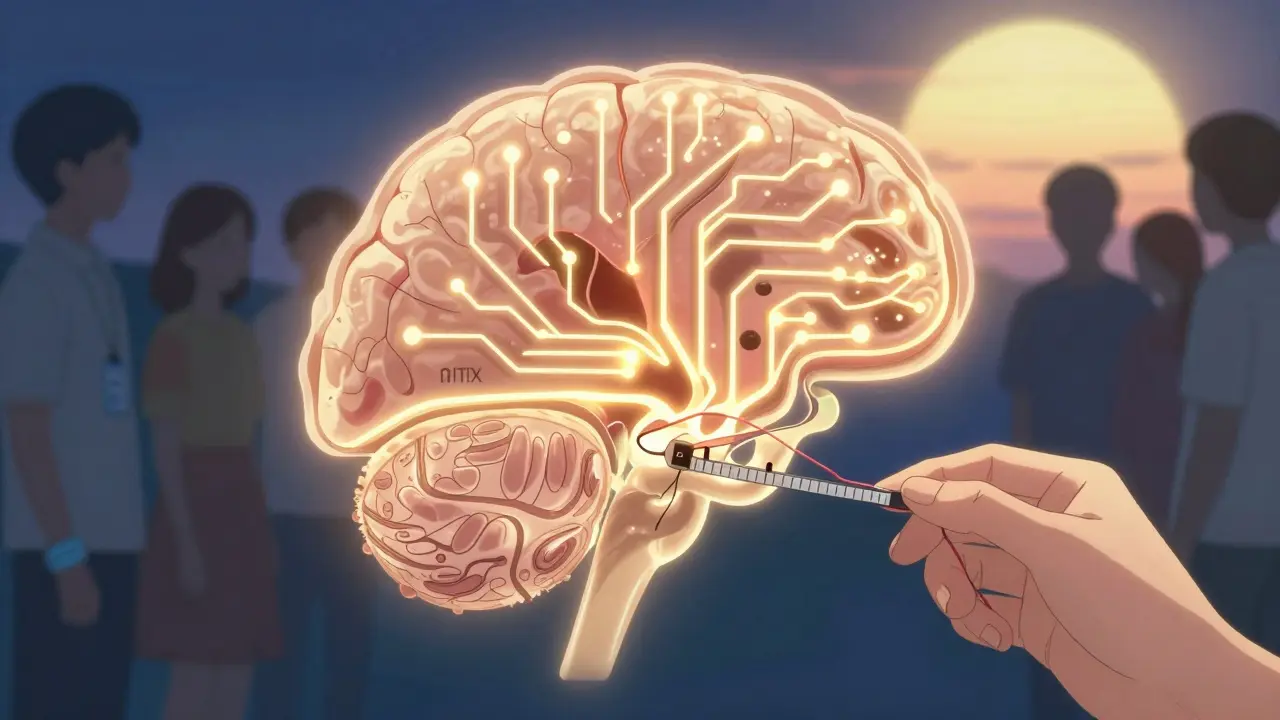
Why Your Body Can’t Handle a Sudden Stop
Your body makes cortisol naturally. It’s the hormone that keeps your blood sugar stable, controls inflammation, and helps you respond to stress-like an infection, injury, or even emotional pressure. When you take synthetic corticosteroids for weeks or months, your brain thinks, “We’ve got plenty of cortisol already,” and shuts off the signal to your adrenal glands. Over time, those glands shrink. They forget how to make cortisol on their own. This isn’t just a problem for people on high doses. A 2023 study in Endocrine Abstracts showed that even low-dose prednisone (less than 5 mg daily) for just four weeks can suppress your adrenal axis. That means someone taking a low-dose steroid for allergies or mild asthma could still be at risk if they stop abruptly. The old rule-that only long-term, high-dose users are at risk-is outdated. The truth is, anyone who’s been on steroids for more than a few weeks needs to taper slowly.What the Symptoms Look Like (And How They’re Often Mistaken)
Symptoms don’t show up right away. They creep in 24 to 72 hours after your last pill. At first, it’s easy to brush them off:- Extreme fatigue-so bad you can’t get out of bed
- Loss of appetite and unexplained weight loss
- Nausea, vomiting, or stomach pain
- Muscle weakness or aching joints
- Mood changes: irritability, depression, or brain fog
- Severe drop in blood pressure
- Dehydration
- Confusion, dizziness, fainting
- Coma or death if untreated
Not All Adrenal Insufficiency Is the Same
There are three types:- Primary: The adrenal glands themselves are damaged (like in Addison’s disease).
- Secondary: The pituitary gland doesn’t make enough ACTH to tell the adrenals to work.
- Tertiary: The hypothalamus stops making CRH, which normally tells the pituitary to act. This is the kind caused by steroid withdrawal.
How Doctors Diagnose It
If you’ve been on steroids and now feel terrible, your doctor should check:- **Morning serum cortisol**-drawn before 9 a.m. Levels below 5 μg/dL are a red flag.
- **ACTH stimulation test**-this is the gold standard. You get a shot of synthetic ACTH, and your cortisol is measured 30 and 60 minutes later. If your cortisol doesn’t rise above 18 μg/dL, your adrenals aren’t responding.
How to Taper Safely-And Why There’s No One-Size-Fits-All
There’s no perfect tapering schedule. But here’s what major guidelines agree on:- If you were on more than 20 mg of prednisone daily for over three weeks-get tested before stopping.
- For doses above 20 mg: reduce by 2.5-5 mg every 3-7 days.
- For doses between 5-20 mg: reduce by 1-2.5 mg every 1-2 weeks.
- If you were on steroids for more than six months, slow it down even more-sometimes over 3-6 months.
What You Need to Do Right Now
If you’re on steroids-or just stopped them-here’s what you must do:- Never stop abruptly. Even if you feel fine. Even if your doctor didn’t mention it.
- Ask for a written taper plan. Don’t rely on memory. Get it in writing.
- Carry an emergency steroid card. The FDA has required this on all systemic steroid packaging since 2021. It tells emergency staff you’re at risk.
- Get trained on emergency hydrocortisone injections. If you feel your symptoms worsening-nausea, dizziness, low blood pressure-give yourself 100 mg of hydrocortisone IM right away. Then call 911. This saves lives.
- Wear a medical alert bracelet. It’s not just for diabetics. If you’ve been on steroids for more than four weeks, this is essential.
What to Do If You Think You’re in Crisis
Adrenal crisis is a medical emergency. If you have:- Severe vomiting or diarrhea
- Low blood pressure or fainting
- Confusion or loss of consciousness
The Bigger Picture: Why This Is Getting Worse
Corticosteroid prescriptions have jumped 23% since 2015. More people are getting them for asthma, arthritis, autoimmune diseases, even long COVID. But awareness hasn’t kept up. A 2023 study in JAMA Internal Medicine found 47% of patients didn’t follow their tapering plan-because they forgot, didn’t understand, or were scared of side effects. The economic cost is heavy: each adrenal crisis hospitalization averages $14,250. And the human cost? Lost work, missed family events, trauma from nearly dying. But there’s hope. AI tools are now being tested to predict who’s at risk by analyzing electronic health records. Point-of-care cortisol tests are in trials-they’ll give results in 15 minutes, right in the doctor’s office. And by 2030, experts predict a 30% drop in adrenal crises thanks to better education and tools.Final Takeaway
Corticosteroids save lives. But they can also kill if stopped the wrong way. You don’t need to be on them for years to be at risk. You don’t need a high dose. The danger is real, silent, and often missed. If you’ve taken steroids in the last six months and feel off-fatigued, nauseous, weak-don’t assume it’s stress or a virus. Ask your doctor: “Could this be adrenal insufficiency?” And if you’re still on them? Ask for a taper plan. Ask for the emergency injection. Ask for the medical alert bracelet. Your life might depend on it.Can adrenal insufficiency happen after just a few weeks of steroid use?
Yes. Even short-term use-like 4 weeks of low-dose prednisone (less than 5 mg daily)-can suppress your body’s natural cortisol production. The old belief that only long-term, high-dose users are at risk is outdated. Research from 2023 confirms that adrenal suppression can occur after just a few weeks, regardless of dose.
What are the first signs of adrenal insufficiency after stopping steroids?
The earliest signs include extreme fatigue (reported in 85% of cases), loss of appetite, nausea, muscle weakness, and mood changes like irritability or depression. These usually appear 24 to 72 hours after your last dose. They’re often mistaken for the flu or burnout, which delays diagnosis.
How do I know if I’m having an adrenal crisis?
An adrenal crisis is a medical emergency. Signs include severe low blood pressure, dizziness or fainting, confusion, vomiting, dehydration, and loss of consciousness. If you have these symptoms after stopping steroids, give yourself an emergency hydrocortisone injection immediately and call 911. Waiting can be fatal.
Do I need to carry emergency steroids even if I tapered slowly?
Yes. Even with a slow taper, some people still develop adrenal insufficiency. The Endocrine Society and FDA recommend that anyone who’s taken systemic steroids for more than four weeks carry an emergency hydrocortisone injection and a medical alert card. Stress events-like infection, surgery, or trauma-can trigger crisis even months after stopping.
Can I test myself for adrenal insufficiency at home?
No reliable at-home test exists yet. Diagnosis requires a blood test for cortisol and ACTH levels, usually done in the morning, followed by an ACTH stimulation test. However, point-of-care cortisol devices are in clinical trials and may become available in clinics soon. Until then, if you suspect adrenal insufficiency, see your doctor immediately.
Are there alternatives to tapering steroids slowly?
There are no proven alternatives to tapering. Some patients try supplements or herbal remedies, but none have been shown to restore adrenal function faster. The only evidence-based method is gradual dose reduction under medical supervision. In some cases, doctors may temporarily replace cortisol with hydrocortisone during the taper if symptoms appear.
How long does it take for the adrenal glands to recover after stopping steroids?
Recovery varies widely. For some, it takes weeks. For others, especially those on long-term therapy, it can take 6 to 12 months or longer. A 2023 study in Nature Medicine found that genetic factors influence recovery speed. There’s no way to predict exactly how long it will take for you. That’s why ongoing monitoring and emergency preparedness are essential.






Katie Schoen
January 6, 2026 AT 22:36Wow. I took a 2-week prednisone pack for a bad cough last year and felt like a zombie for a month after. My doctor never mentioned tapering. I thought I was just ‘burnt out.’ Turns out my adrenals were on vacation. Thanks for this. I’m getting my emergency card now.
Also, why is it that the scariest medical facts come from Reddit threads and not pamphlets from the pharmacy?
Beth Templeton
January 7, 2026 AT 02:55Low dose still kills you. Done.
Ryan Barr
January 8, 2026 AT 22:30Adrenal suppression isn't even a real clinical entity in most endocrinology textbooks-it’s just a euphemism for iatrogenic HPA axis dysfunction. The fact that laypeople are now calling it ‘adrenal fatigue’ is why medicine is collapsing. If you’re not measuring ACTH and cortisol at 8 a.m., you’re just guessing.
And no, hydrocortisone isn’t a ‘supplement.’ It’s a glucocorticoid. Learn the terminology before you panic.
Dana Termini
January 9, 2026 AT 00:06I’m a nurse and I’ve seen this too many times. Patients come in confused, weak, dehydrated-and they swear they ‘just stopped the pills because they felt fine.’
It’s heartbreaking. No one ever tells them this could happen. We need better discharge instructions. Like, printed. In bold. With a checklist.
And yes, I give out emergency cards now. No exceptions.
Wesley Pereira
January 9, 2026 AT 12:31So let me get this straight-we’re telling people to carry an EpiPen for their own adrenal glands? That’s wild. And kinda genius.
Also, the fact that 47% of folks don’t taper properly? That’s not negligence. That’s systemic failure. Doctors are overworked. Patients are overwhelmed. And the system just… drops the ball.
But hey, at least we’ve got AI tools coming. Maybe by 2030, your phone will auto-schedule your taper and text you when to inject. Until then? Don’t be the guy who Googles ‘why do I feel like dying after steroids’ at 2 a.m.
Get the card. Get trained. Don’t be a statistic.
Rachel Wermager
January 10, 2026 AT 04:07Primary vs. secondary vs. tertiary adrenal insufficiency is critical to distinguish because the ACTH dynamics dictate management. Tertiary is hypothalamic-pituitary suppression-so ACTH is low, cortisol is low, and stimulation tests are blunted. Primary is Addison’s-ACTH sky-high, cortisol low, and the adrenal cortex is toast.
Most clinicians still confuse tertiary with secondary. This leads to inappropriate dexamethasone suppression testing and misdiagnosis. If your ACTH is <5 pg/mL and cortisol is <5 μg/dL, it’s steroid-induced. Period.
Katelyn Slack
January 11, 2026 AT 23:40i just got off prednisone after 6 weeks for my asthma and i’ve been so tired i thought it was covid again. i didn’t know it could be this bad. i’m gonna ask my doc for a card and a plan. thanks for posting this. i almost ignored it cause i thought it was scaremongering but… yeah. nope.
also i think i spelled ‘adrenal’ wrong in my notes. oops.
Molly McLane
January 13, 2026 AT 17:11If you’re reading this and you’ve ever been on steroids-even for a week-please don’t ignore this. I’ve had patients who thought they were ‘fine’ after stopping… until they collapsed at the grocery store.
It’s not about fear. It’s about preparation. Like wearing a seatbelt. You don’t think you’ll crash. But if you do, you’re glad you did it.
Ask for the card. Ask for the training. Ask for the bracelet. It takes 5 minutes. Could save your life.
And if you’re a provider? Don’t assume they know. Write it down. Say it twice. Make them repeat it back.
Harshit Kansal
January 15, 2026 AT 02:10Bro. I took steroids for a rash. One week. Then I stopped. Felt like I was dying for 3 days. Went to the ER. They thought I was faking. I was like ‘I’m not high, I’m just… out of cortisol.’
They finally tested me. Low cortisol. Low ACTH. They gave me IV hydrocortisone and I cried. Not because I was weak. Because no one told me this could happen.
Now I tell everyone. This isn’t a ‘maybe.’ It’s a ‘when.’
Matt Beck
January 16, 2026 AT 11:49Think about it: our bodies evolved to handle fire, famine, predators… not pharmaceuticals. We’ve hijacked our own endocrine system with synthetic molecules, then wonder why it breaks down.
Adrenal insufficiency isn’t a disease-it’s a rebellion. Your HPA axis, your ancient, beautiful, 500-million-year-old stress-response system… it’s saying: ‘I didn’t sign up for this.’
So we don’t just need tapering protocols-we need humility. We need to remember that biology isn’t a dial we can turn up and down at will. We’re guests in our own bodies.
And if you’re reading this? You’re one of the lucky ones. You’re awake.
Now go get that card. 🌱