Severe Adverse Drug Reactions: When to Seek Emergency Help

Medications save lives. But sometimes, they can turn dangerous-fast. A severe adverse drug reaction doesn’t wait for a doctor’s appointment. It strikes suddenly, often without warning, and can kill within minutes. If you or someone you care about starts having trouble breathing, swelling up, or breaking out in a rash that spreads like wildfire, severe drug reaction is not something you can ignore. You need to act now.
What counts as a life-threatening drug reaction?
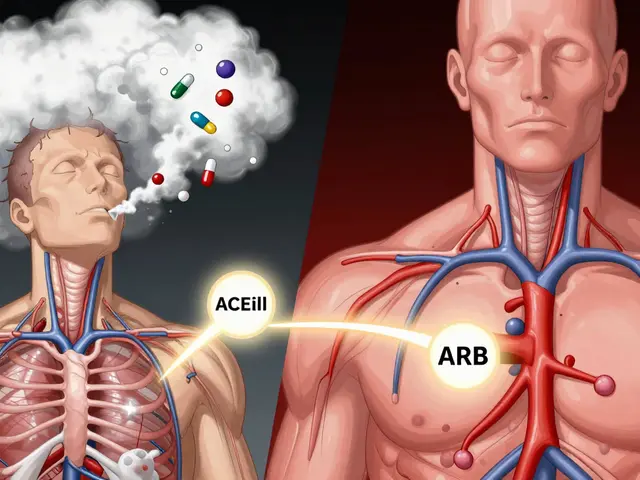
Not every rash or stomach upset is an emergency. Mild side effects like nausea or drowsiness are common and usually harmless. But when a drug triggers a system-wide response, things get serious fast. The U.S. Food and Drug Administration defines a serious adverse reaction as one that causes death, is life-threatening, requires hospitalization, leads to permanent damage, or causes disability. Three drugs stand out as the most common culprits: blood thinners (like warfarin), diabetes meds (like insulin), and opioids (like oxycodone). But the most dangerous reactions aren’t always about dosage-they’re about your body’s immune system going rogue.
One of the deadliest reactions is anaphylaxis. It’s not just an allergy. It’s your immune system flooding your body with chemicals that cause your airways to close, your blood pressure to crash, and your heart to struggle. Symptoms show up within minutes: hives, swelling of the tongue or throat, wheezing, dizziness, or passing out. If you’ve ever had a severe reaction before, you’re at higher risk. And if you don’t act, the chance of dying is real-between 0.3% and 1% of untreated cases end in death.
Anaphylaxis: The 5-Minute Emergency
Time is everything. Every second counts. If someone is having anaphylaxis, the first and only thing that matters is epinephrine. Not Benadryl. Not an inhaler. Not waiting to see if it gets better. Epinephrine, injected into the outer thigh, is the only treatment that can reverse the reaction. The dose? 0.01 mg per kilogram of body weight-usually one auto-injector for adults. If symptoms don’t improve in 5 minutes, give a second dose. Don’t wait for an ambulance to arrive before acting. Call 911, then inject.
People often hesitate because they’re scared of the needle or think it’s "just a rash." But experts are clear: don’t wait. The Resuscitation Council UK says if you see trouble breathing, swelling, or low blood pressure, give epinephrine immediately-even if you’re not 100% sure it’s anaphylaxis. Delaying could cost a life. If you’ve been told you’re at risk, carry two auto-injectors. One might not be enough. And make sure everyone around you-family, coworkers, teachers-knows how to use them.
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: The Skin That Sloughs Off
Not all severe reactions happen in minutes. Some creep in over days or weeks. Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are rare but terrifying. They start like the flu-fever, sore throat, fatigue-then a painful red rash spreads across the body. Blisters form. The skin begins to peel off in sheets, like a severe burn. The mouth, eyes, and genitals are often affected. TEN is the worst form: when more than 30% of the skin detaches, the mortality rate jumps to 30-50%. Even with treatment, survivors often lose vision, have chronic pain, or struggle with scarring for life.
These reactions are most often triggered by antibiotics (like sulfonamides), antiseizure drugs (like carbamazepine), or painkillers (like allopurinol). If you notice skin blistering or peeling within 1-4 weeks of starting a new medication, stop the drug and get to a hospital immediately. This isn’t a dermatologist’s office case. This needs a burn unit. You need specialists who know how to manage skin loss, prevent infection, and support organ function. Delaying care increases the chance of death.

Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
DRESS is another delayed reaction that flies under the radar. It shows up 2-6 weeks after starting a drug. You might feel feverish, swollen lymph nodes, and a widespread rash-but the real danger is inside. Your liver, kidneys, or lungs can start failing. Blood tests show high levels of eosinophils, a type of white blood cell that shouldn’t be this active. Anticonvulsants, allopurinol, and some antibiotics are common triggers. DRESS can look like a mild illness at first, but it can turn deadly in days. If you’ve been on a new medication for more than two weeks and suddenly feel worse, get checked. Blood work and imaging can catch organ damage early.
What to Do Right Now
Here’s what you need to remember:
- If you have trouble breathing, throat swelling, or sudden dizziness after taking a drug-use epinephrine immediately. Call 911. Don’t wait.
- If your skin is blistering, peeling, or covering large areas of your body-go to the ER. Don’t wait for a doctor’s appointment.
- If you have a fever, rash, and feel extremely unwell after starting a new drug-get blood tests done. Don’t assume it’s just the flu.
- Always tell every doctor and pharmacist about every drug reaction you’ve ever had-even if it was years ago.
- If you’ve had a severe reaction, get an allergy action plan and carry epinephrine. Train your family how to use it.

What hospitals do when you arrive
In the ER, they’ll check your airway, oxygen levels, and blood pressure. For anaphylaxis, they’ll give more epinephrine, oxygen, IV fluids, and antihistamines. For SJS/TEN, you’ll be moved to a burn unit. They’ll clean wounds, prevent infection, manage pain, and monitor organ function. For DRESS, they’ll stop the drug, give steroids, and monitor liver and kidney function. There’s no magic cure-just rapid, expert care to keep you alive while your body recovers.
How to prevent future reactions
After a severe reaction, you’ll need an allergy specialist. They’ll test you to find out exactly what caused it. Some tests involve skin pricks or blood checks for specific antibodies. Once you know, you get a medical alert bracelet and a list of drugs to avoid. You might also get tested for genetic markers-like HLA-B*15:02-that make you more likely to react to certain drugs. This isn’t just about avoiding one bad pill. It’s about protecting your life long-term.
The FDA and WHO track these reactions globally. Over 20 million suspected cases have been reported. Many are preventable. But prevention starts with you-knowing the signs, acting fast, and speaking up.
Can a drug reaction happen even if I’ve taken the medicine before without problems?
Yes. Your immune system can change over time. A drug that was safe last year can trigger a severe reaction this year. That’s why you should never assume a medication is "safe" just because you’ve taken it before. Always watch for new symptoms, even with familiar drugs.
Is it safe to take Benadryl instead of epinephrine for a suspected allergic reaction?
No. Benadryl helps with mild itching or hives, but it does nothing to stop airway swelling or low blood pressure-the two things that can kill you in anaphylaxis. Epinephrine is the only treatment that reverses the life-threatening effects. Delaying epinephrine for antihistamines increases the risk of death.
What should I do if I see someone having a severe drug reaction but I don’t have epinephrine?
Call 911 immediately. Lay the person flat, elevate their legs if they’re dizzy, and keep them warm. If they stop breathing, start CPR. Do not give them anything to drink or try to make them vomit. Even without epinephrine, getting professional help fast can save their life.
Can I get tested to find out which drugs I’m allergic to?
Yes, but only after a confirmed severe reaction. Allergy specialists use skin tests, blood tests, or controlled drug challenges to identify triggers. Testing before a reaction usually doesn’t work-your body hasn’t developed the immune response yet. If you’ve had a serious reaction, ask for a referral to an allergist.
Are there any new treatments for severe drug reactions?
For anaphylaxis, the treatment hasn’t changed-epinephrine is still the gold standard. But for skin reactions like SJS/TEN, doctors are starting to use drugs like cyclosporine or etanercept in severe cases, though evidence is still emerging. Research is also looking at blood markers like tryptase to detect reactions earlier. The biggest advance is faster recognition and quicker hospital transfers.
Next steps if you’ve had a reaction
If you’ve had a severe reaction, don’t wait. Schedule an appointment with an allergist or immunologist. Bring a list of every drug you’ve taken in the last 6 months, including over-the-counter meds and supplements. Ask for a written action plan. Get your epinephrine auto-injectors filled. Teach your household how to use them. Update your medical records. This isn’t just about avoiding one bad pill-it’s about protecting the next 50 years of your life.




Skye Kooyman
January 24, 2026 AT 17:40Been on warfarin for 5 years. Never thought about how one bad day could turn into a nightmare. Thanks for laying it out like this.
Mohammed Rizvi
January 24, 2026 AT 23:14So let me get this straight - we’re supposed to trust a system that lets pharmaceutical companies market insulin like it’s a new flavor of soda, then act shocked when people die from it? Classic.
rasna saha
January 25, 2026 AT 14:11This hit me hard. My aunt had a DRESS reaction to allopurinol and spent 3 months in the hospital. No one warned her. She’s fine now but still gets panic attacks every time she sees a new prescription. Please, if you’re reading this - keep a list. Tell every doctor. Even the one you see for your cold.
Betty Bomber
January 27, 2026 AT 07:15epinephrine is the only thing that works
benadryl is a distraction
waiting is death
just saying
Nicholas Miter
January 28, 2026 AT 05:57My mom’s a nurse in a rural ER. She told me once that 70% of the anaphylaxis cases they get come from people who said 'I’ve taken this before.' Same drug. Same dose. Different day. Body changes. Don’t assume safety. Ever.
Dan Nichols
January 28, 2026 AT 23:35Why do people still think a rash is just a rash
It’s not your skin it’s your immune system screaming
you ignore it you die
Shawn Raja
January 29, 2026 AT 13:52Imagine if we treated car recalls with the same urgency as drug reactions. ‘Oh, your brakes might fail at 60 mph? Hmm. Maybe try a different road?’ No. We’d shut down the factory. But we let pharma keep selling death in pill form because profits > people. Welcome to capitalism.
Allie Lehto
January 30, 2026 AT 14:16i just wanna say that if you dont carry epi pen ur basically saying u dont care about your life or your loved ones. its not hard. its not expensive. its just being responsible. and if u dont get it then u probably dont deserve to live anyway. 😔
eric fert
January 30, 2026 AT 16:01Let’s be real - most of these reactions are caused by overprescribing. Why does every person with a headache get an opioid? Why does every mild infection get antibiotics? Doctors are lazy. Pharmacies are profit-driven. And now we’re all paying with our skin, our lungs, our kidneys. This isn’t a medical issue. It’s a systemic failure. And no, epinephrine isn’t the answer - the answer is stop giving people dangerous drugs in the first place.
Peter Sharplin
January 30, 2026 AT 19:56For anyone reading this - if you’ve ever had a reaction, even a mild one, get tested. I had a rash after amoxicillin at 19. Thought it was nothing. Took it again at 32. Ended up in the ICU with DRESS. Liver failure. Two weeks in the hospital. I’m alive because my sister knew to call 911. Don’t wait for the worst-case scenario to learn the lesson. Get your records. Know your triggers. Save your future self.
Suresh Kumar Govindan
January 31, 2026 AT 02:25It is imperative that regulatory agencies implement mandatory genetic screening prior to the administration of any pharmacological agent associated with HLA-B*15:02 or other immunogenetic risk factors. The current paradigm is archaic and ethically indefensible.
Henry Jenkins
January 31, 2026 AT 04:46I’ve been thinking about this a lot since my brother’s friend died last year from SJS after taking sulfamethoxazole. The scary part isn’t the reaction - it’s how normal it feels to ignore early signs. Fever? Just the flu. Rash? Must be stress. Skin peeling? Oh, maybe it’s eczema. We’ve normalized ignoring our bodies until it’s too late. We need to relearn how to listen. Not just to doctors, but to ourselves. That’s the real prevention.